
Eczema refers to a group of conditions that cause inflammation of the skin. There are many types of eczema. Atopic dermatitis is the most common type. Other types of eczema include seborrheic dermatitis, which often coexists with blepharitis/dry eyes, contact dermatitis, nummular eczema, and dyshidrotic eczema. Doctors often refer to eczema as any of these conditions.
Eczema is a skin condition that causes dry, itchy patches of skin. It is a common condition that is not contagious. Eczema symptoms can flare up if you come into contact with an irritant or allergen.
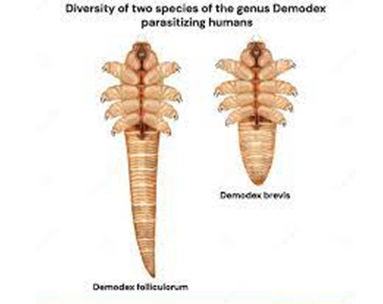
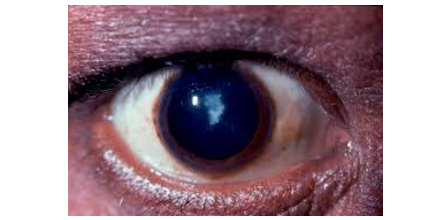
Bacteria and Demodex parasites are key causative factors of eczema and dermatitis on the face & eyes.
Demodex bacteria and parasites on the skin of the face and eyelids are a common cause of eczema, blepharitis and tear film destabilization resulting in dry eyes, blurred vision and reduced quality of life. It is known and scientifically proven that too many Demodex bacteria and parasites on the eyelids due to ignorance of eyelid/eyelash hygiene, can cause inflammation, irritation and chronic dry eyes. For this reason, eyelid/eyelash hygiene with Ophthalmogen & Naviblef products is particularly important.
Dermo-Ophthalmology – The new integrated Skin-Eyelid-Ocular Surface approach
In recent years, the scientific community has recognized that the skin, eyelids, Meibomian glands, and tear film constitute a single functional system. Δερμοφθαλμολογία (Dermophthalmology) is the emerging field that organizes and systematizes this contemporary knowledge. This approach explains why eczema – even when it starts on the skin of the face – can: • destabilize the tear film, • cause blepharitis, • affect the Meibomian glands (MGD), • lead to blurred vision & reduced comfort. More about the scientific context of Dermophthalmology: Dermophthalmology Official Website Dermophthalmology – Position Papers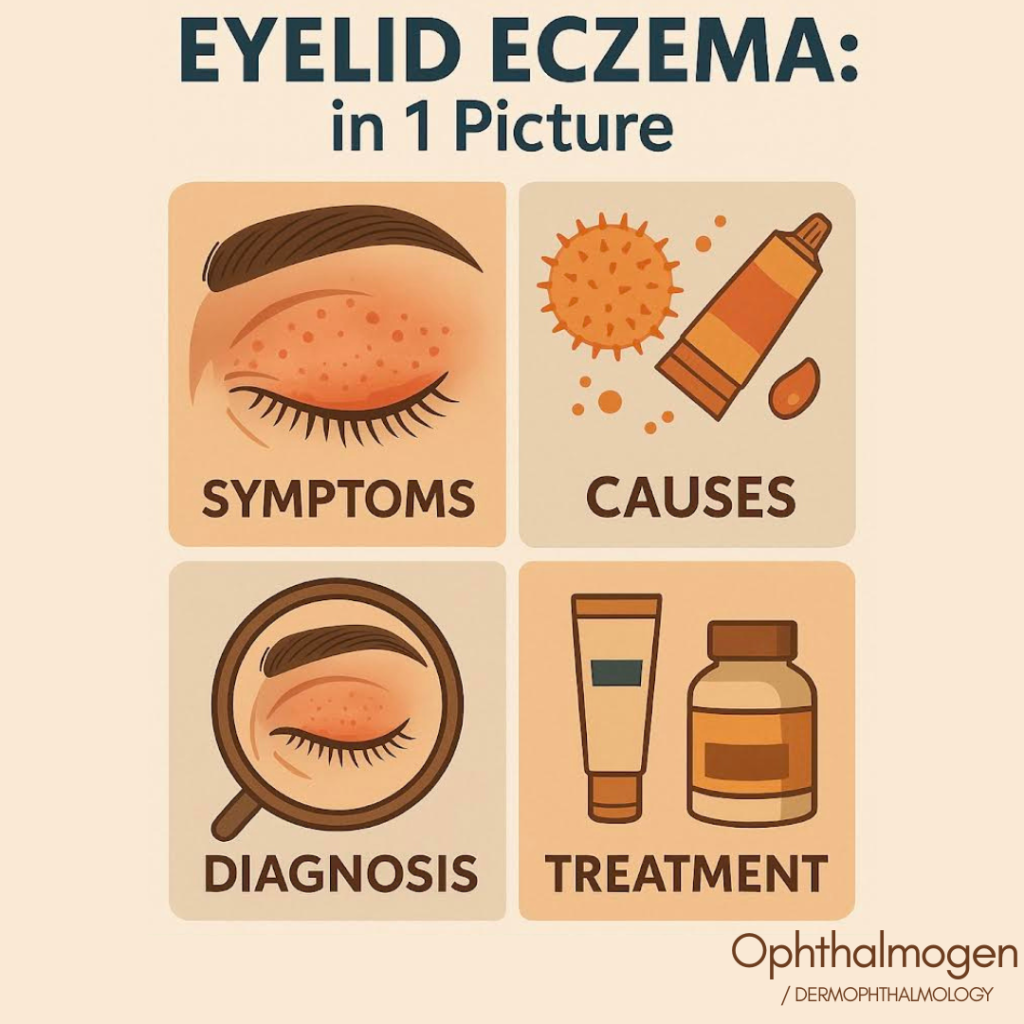

What are the types of eczema according to the National Eczema Association?
There are 7 types of eczema that can appear either on the skin of the face or on the skin of the eyes (eyelids) which is even more sensitive:
– Atopic dermatitis
– Contact dermatitis
– Seborrheic dermatitis
– Dyshidrotic dermatitis
– Neurodermatitis
– Numbing eczema
– Stasis dermatitis
Risk Factors
- Family history of eczema, blepharitis/dry eyes, asthma, or hay fever.
- Sensitive skin.
- Working in an environment where you are exposed to harsh chemicals or fumes.
- A weakened skin barrier or a history of epidermal inflammation.
- Aminoglycoside antibiotics can cause blepharodermatitis.
- Atropine eye drops commonly cause contact dermatitis.
- A variety of bacteria, parasites, fungi, and viruses can cause infected eczema. Some of the most common germs, parasites, and fungi responsible for causing eczema are:
Staphylococcus aureus, Demodex parasites, Bacillus oleronius, Staphylococcus epidermidis, Malassezia fungus, Candida albicans
- Stress, climate change, increased exposure to skin irritants, dry skin, diet, and glaucoma medications can all contribute to the sudden onset of eczema in adulthood. According to American dermatologist Dr. Rogge, our skin becomes drier as we age and loses its normal lipid barrier, and hormonal changes may also play a role.
- Preservatives used in contact lens solutions.

Eyelids: The sensitive skin of the eye
The skin of the eyelids is 4 times thinner than the skin of the face.The skin of the eyelids, being so thin, is particularly sensitive to irritants and allergens and therefore prone to developing contact dermatitis.
Why do I have contact dermatitis?
The eyelids are complex structures made up of muscles and nerves, all covered by a thin layer of skin called the epidermis. The skin on the eyelids is thinner than that on the rest of the body, making it more prone to irritation, and inflammation in this area is known as blepharitis and blepharodermatitis.

What is Seborrheic Dermatitis?
Seborrheic dermatitis is a common, chronic, relapsing, inflammatory skin disorder of both the face and eyelids.The cause of the disease is not fully understood. Recent scientific studies indicate that parasites regulation play a role in the etiopathogenesis of seborrheic dermatitis.
Considered as chronic form of eczema, seborrheic dermatitis appears on the eyelids, face, and body where there are many sebaceous glands which produce the fatty substance – oil. Most sebaceous glands are located in the eyes, the nose, the scalp and the upper back.
Η σμηγματορροϊκή δερματίτιδα ονομάζεται επίσης πιτυρίδα, σμηγματορροϊκό έκζεμα και σμηγματορροϊκή ψωρίαση. Όταν εμφανίζεται σε βρέφη ονομάζεται cradle cap.
The unique skin of the eyes
The eyelids are the thinnest skin on the body, 0.55nm, thus allowing easier penetration of allergens. In fact, the eyelids may manifest as the initial or only site of allergic contact dermatitis symptoms, even with allergen exposure occurring elsewhere on the body..

Rubbing your eyes with painted nails can cause irritation.
A common cause of contact dermatitis of the eyelids is an allergy to nail polish. The skin of the eyelids becomes sensitive when you touch or rub your eyes with painted nails.For this reason, it is recommended that those who use makeup and professional makeup artists spray the eyelids with the Spray της Ophthalmogen.

Irritant contact dermatitis is the result of irritants such as makeup, detergents, shampoos, or solvents coming into contact with the eyelids and then damaging and irritating the skin. Anti-aging cosmetics that come into contact with the skin of the eye can also cause irritation.
Also, some medications can cause contact dermatitis. If your eyelid eczema does not improve or control with eyelid hygiene treatment, you should ask for a referral to an ophthalmologist because the health of the skin of the eye can affect vision.
Parasite infection is common regulation on the eyelids and face
Keep in mind that the skin around the eyes can be infected with parasites. regulation (demodectic mange) and bacteriaIf your eyes water or develop a golden crust (bacterial infection/demodectic mange) or small fluid-filled blisters (viral infection called eczema herpeticum), seek eye care.
Blepharitis is directly linked to dermatitis
Inflammation of the eyelids leads to itching and discomfort, as well as the feeling that there may be something "hairy" on the surface of the eyes. The most important treatment was, is and will be good eyelid hygiene.This involves the use of a 40C warm, disposable self-heating compress such as Ophthalmogen Eye10 or the multi-purpose Eyegiene.
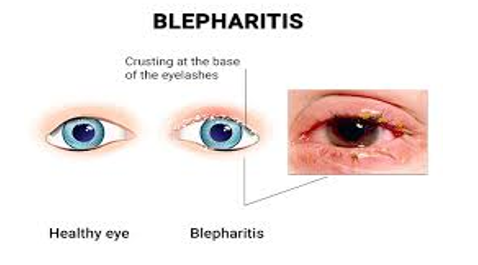
After using the self-heating compress, it is necessary to gently massage the eyelids in a circular motion to unblock the oil glands (meibomian glands) in your eyelids. The eyelid massage is done with Ophthalmogen gel (ointment for Demodex inflammation).
In many cases where you may wake up with puffy eyes and eyelids stuck together, what you need to do is wash your eyelids with Naviblef Daily Care and warm water and then spray them with Ophthalmogen Spray.
Artificial tears can be used to moisten the cornea (the outer surface of the eye), making your eyes more comfortable. It is a good idea to stop wearing contact lenses and use hypoallergenic eye makeup, as these can further irritate blepharitis. Your pharmacist should refer you to an ophthalmologist for an accurate diagnosis of your condition.


- 46% of blepharitis patients suffer from seborrheic dermatitis

Why do I suddenly have eczema on my eyelids?
Around the eye or on the eyelids, eczema is very common. Eye eczema can be caused by allergies, antiglaucoma eye drops, or it can be one of the many possible manifestations of atopy (along with asthma), a genetic hypersensitivity to the environment..
Reduce immediate allergic eyelid discomfort with Ophthalmogen constant controlled cooling cool compresses and antihistamines to reduce mild allergic reactions. In any case, "Stop rubbing your eyes when they are itchy because it can deform your cornea and cause keratoconus," say the world's best ophthalmologists.
The ideal way, besides medication, to stop itchy eyes is by massaging the eyelids with Ophthalmogen products gel or spraying them with Ophthalmogen products SprayMany patients who suffer from itchy eyes have found an easy solution to their problem by innovatively spraying their eyelids/eyelashes with Ophthalmogen spray.
What is peri-ocular dermatitis?
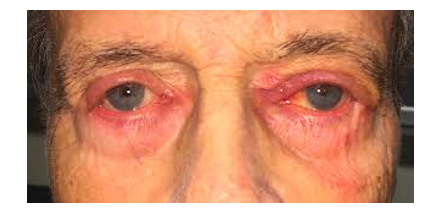
Periorbital dermatitis, also known as periorbital dermatitis, is a common dermatological disorder characterized by inflammation of the eyelids and skin surrounding the eyes.
Periorbital dermatitis is a common skin problem and occurs in 3.9-4.8% of patients presenting for patch testing.

Peri-ocular dermatitis from cosmetics
Women are affected more often than men, accounting for 73-80% of cases.This difference has been attributed to the use of cosmetic products, which is more common in women. The single most common cause of periorbital dermatitis is allergic contact dermatitis, which can be attributed to 31-72% of cases. The 14-39.5% of cases are due to atopic dermatitis. Irritant contact dermatitis is only the 7-9% – percentage which contrasts with the body as a whole, in which irritant contact dermatitis is responsible for 70-80% of all causes of contact dermatitis. Among the most common causes of contact dermatitis affecting the eyelids is the use of hair dye, especially those containing phenylenediamine.
Can eye drops cause eczema on the eyelids?
Some medications can cause contact dermatitis. For this reason, after instilling eye drops, we should treat our eyelids and eyelashes with Ophthalmogen Spray & Wipes to prevent the risk of allergic inflammation.
Can glaucoma eye drops cause skin irritation?
Your glaucoma specialist will tell you that the ocular and periocular dermatological side effects of glaucoma eye drops are contact dermatitis, hyperpigmentation, prostaglandin analog periorbitopathy, mucous membrane pemphigoid, eyelash discoloration, skin hypertrichosis, and rare cases of melanoma and skin discoloration.
Most of the cutaneous side effects of glaucoma eye drops are ocular and peri-ocular and are caused by prostaglandin analogues. Furthermore, topical beta-blocker eye drops used to treat glaucoma are known to cause peri-ocular dermatitis, and brimonidine eye drops are another common cause of peri-ocular dermatitis. For this reason, do not forget to spray your eyelids with Ophthalmogen Spray before/after anti-glaucoma treatment as a compensatory measure.
Can antibiotic eye drops cause a skin rash?
Side effects of antibiotic eye drops may be common, occasional, or rare. Mild side effects include itchy eyes, red eyes, inflamed eyes, contact dermatitis, and skin rash.. Among the rare effects are blurred vision, eye pain, eye irritation, headache and iritis. For this reason, after instilling eye drops in the eyes, we should treat our eyelids and eyelashes with Ophthalmogen wipes/Spray/gel in order to prevent any negative effects of the drugs, which are also listed in their instructions.
What is the connection between Atopic Dermatitis and the eyes?
Eye problems can be a reality for anyone living with Atopic Dermatitis, the most common type of eczema. Atopic Dermatitis can develop on your eyelids and around your eyes, causing itchy, flaky eyelid skin and red, swollen eyes. Incorporating daily eyelid/eyelash hygiene into your routine will help you feel more comfortable and possibly improve the quality of your vision.

- Up to 50% of patients with atopic dermatitis may suffer from blepharitis/dry eye
- 25-50% of patients with atopic dermatitis may suffer from blepharitis/dry eye, conjunctivitis, tear film disorders, keratoconus, uveitis, cataracts, retinal detachment. Atopic dermatitis is not a single disease entity that affects only the skin but coexists with disorders of other organs at the same time..

Bacteria and atopic dermatitis
Control the pest population regulation & βακτηρίων στο δέρμα σας
The frequency of bacterial colonization in the conjunctival sacs of the eye and at the eyelid margins in patients with atopic dermatitis is clearly higher compared to individuals without atopic dermatitis (86% vs. 25%). Especially the Staphylococcus Aureus has been detected in 67% of patients with atopic dermatitisFor this reason, it is necessary for sufferers of atopic dermatitis to integrate eyelid and facial hygiene with special pharmaceutical products such as Ophthalmogen, Naviblef in order to control the population of bacteria, Demodex parasites and inflammation.
Keratoconus and atopic dermatitis
Main patients with atopic dermatitis they may have higher risk of developing keratoconus, according to research presented at the annual meeting of the ARVO–Association for Research and Vision in Ophthalmology in Seattle, America, May 5-9, 2024.
The connection between keratoconus and atopy has been described by Hilgartner already since 1937.

- 1977 an article in British Journal of Ophthalmology revealed that the 35% of patients with keratoconus had atopic tendencies (hay fever was the most common, but also asthma and eczema), while in the healthy control group, only the 12% of patients showed such tendencies.
- 75% of keratoconus patients who underwent Cross–Linking also had allergic conjunctivitis
Because based on scientific data The health of facial skin is directly related to the health of the eyelid skin and the quality of vision., patients suffering from atopic dermatitis should closely follow the instructions of their dermatologist and ophthalmologist. The ophthalmologist will monitor the condition of the patient's eyelids/eyelashes, eyes and vision and will contribute to improving the quality of life and preventing the appearance of keratoconus.
Retinal detachment in atopic dermatitis
19.2% is the estimated incidence of retinal detachment in patients with atopic dermatitis. We can suspect retinal detachment in people with atopic dermatitis when the pigmentation in the anterior chamber corner of the eye is moderate to dense.
Cataracts and atopic dermatitis
Posterior subcapsular cataract is a recognized complication of atopic dermatitis in adults. Cataracts in patients with atopic dermatitis are usually bilateral, symmetrical, and occur in the posterior and anterior subcapsular regions. Its progression depends on factors such as eye rubbing and the severity of facial skin lesions..
Sasabe et al. demonstrated an association between high serum IgE levels and cataract development in individuals with atopic dermatitis. A study in the Danish population revealed association between cataracts and atopic dermatitis only in patients under 50 years of age.
People with atopic dermatitis should be examined regularly by an ophthalmologist., regardless of the dermatological severity of atopic dermatitis, as ocular complications may occur despite mild skin changes.
Cataracts may be due to atopic dermatitis but may also occur secondary to the use of corticosteroids..
The most serious complications of atopic dermatitis are::
- Hydroponic keratitis
- Infection after eye surgery
- Retinal detachment
- IOL dislocation
Children in particular should undergo an ophthalmological examination as soon as the diagnosis of atopic dermatitis is established, as ocular manifestations can progress rapidly and early detection will facilitate early diagnosis and appropriate treatment to avoid permanent ocular damage.
Glaucoma and atopic dermatitis
The relationship between atopic dermatitis and glaucoma has been frequently reported since Harris first suggested glaucoma as an adverse effect of glucocorticoid therapy in 1960. Many studies have reported a positive association between glaucoma and atopic dermatitis.Steroid use has often been suggested as the single most important cause of glaucoma development in patients with atopic dermatitis.


Dry eye and atopic dermatitis
Dry eye has been suggested as a related symptom of atopic keratoconjunctivitis, which is a serious ocular complication in patients with atopic dermatitis. Abnormal tear function, including meibomian gland dysfunction and reduced tear film breakup time, have been proposed as the main pathogenic mechanisms involved in the development of irritation and dry eye, which are directly treated with the use of Ophthalmogen Eye10 self-heating compresses and eyelid massage with Ophthalmogen Gel.
Do I have psoriasis or eczema?
Dr. Palmer explained that eczema is typically “characterized by poorly demarcated red, dry areas with fine scaling,” while psoriasis appears as “red, well-circumscribed lesions called plaques, with accumulated white scaling.” Skin infections are common in people with eczema and can cause odors. When the skin barrier and tear film in the eyes are damaged, bacteria and other microorganisms and invaders can enter, causing various types of infections.For this reason, the eyes of these patients should be sprayed daily with Ophthalmogen Spray.

Improve the protective capacity of the eyelids
When the barrier function of the skin is weak, the skin is less able to retain moisture and protect against bacteria, Demodex parasites, irritants, allergens and environmental factors. Improving the water retention capacity of the eyelid skin can be achieved with the advanced long-lasting moisturizing formula of Ophthalmogen gel/spray which, at the same time as its mild antibacterial & anti-Demodex action, balances the skin flora.
Dermatitis Treatment
(1) You must avoid rubbing your eyes at all costs::
Α) Massage your eyelids daily with Ophthalmogen gel with beneficial soothing, moisturizing, anti-allergic effects, which reduce your need to rub your eyes.
Β) Spray your eyelids during the day wherever you are, with Ophthalmogen spray which is extremely effective.
(2) How to clean your eyes::
Α) Wash your eyelids with Naviblef Daily Care foam once a day.
Β) Wash your face and eyelids with Ophthalmogen 2 in 1 foam if you have sensitive eyes and suffer from some skin disease on your face.
(3) How to moisturize the ocular surface of your eyes
Α) The best and easiest way to moisturize your eyes is undoubtedly spraying your eyes. Use the 1stο artificial tear in spray form Flora Vision spray. The spray has the advantage that you can spray it directly on open eyes, anywhere and anytime, without the restriction of clean hands and the risk of infection.
Β) Artificial tears in the form of eye drops/ampoules such as the latest generation multivitamin Visionlux Plus/Navitae Plus are ideal for use in severe forms of blepharitis/dry eye.
(4) How to get rid of unsightly redness on the ocular surface
Α) Use herbal eye drops or sprays such as Navi Infla eye drops or Flora Vision Spray Red Eyes and avoid rubbing your eyes with the instructions given to you in (1).


(Dermophthalmology Evidence Block – Ophthalmogen Edition)
Modern literature confirms that eyelid eczema, blepharitis, Meibomian gland dysfunction (MGD) and dry eyes constitute a single pathophysiological spectrum — the Ophthalmo-Dermal axis, as defined by Dermophthalmology.
Below are 7 fundamental studies that support the clinical and therapeutic directions of the article:
Study 1 — Malassezia & Eyelid Inflammation
Journal of the European Academy of Dermatology & Venereology, 2020:Showed that Malassezia plays a key role in the creation of inflammation in the eyelids, especially in patients with seborrheic dermatitis and eczema.
Study 2 — Seborrheic Dermatitis & MGD Connection
Cornea Journal, 2019: A study in 214 people showed that 72% of patients with seborrheic dermatitis had Meibomian Gland Dysfunction, leading to blurred vision & dry eyes.
Study 3 — Biofilm & Chronic Eyelid Inflammation
Clinical Dermatology, 2021Showed that the formation of biofilm at the roots of the eyelashes increases inflammation by 28%, directly affecting both the skin and the tear film.
Study 4 — Eyelid Skin Barrier Dysfunction
British Journal of Ophthalmology, 2017: Eyelid skin barrier dysfunction leads to high rates of contact dermatitis, eczema flares, and tear film disorders.
Study 5 — Demodex, Eczema & Blepharitis
Ocular Surface, 2021: Patients with eczematous dermatitis have an overpopulation of Demodex, which is associated with:
– blepharitis
– MGD
– χρόνια ξηροφθαλμία
– συχνά χαλάζια
(→ Confirms the use of Ophthalmogen gel/spray)
Study 6 — Atopic Dermatitis & Ocular Surface Damage
American Journal of Ophthalmology, 2020:Up to 50% of people with atopic dermatitis experience:
– dry eyes
– blepharitis
– eyelid inflammation
– keratoconus when rubbing their eyes
Μελέτη 7 — Seborrheic Dermatitis & Tear Film Instability
Journal of Ophthalmic Inflammation and Infection, 2022: Demonstrated that eyelid peridermatitis leads to tear film destabilization in less than 48 hours.
Dermophthalmology Framework (WOD Global)
Οι παραπάνω μελέτες εντάσσονται στο πλαίσιο της νέας Δερμοφθαλμολογίας:
Dermophthalmology recognizes that the eyelid skin + MGD + tear film constitute a common target organ.
Ophthalmogen 3-Step Protocol (EYE10 – Gel – Spray)
(Scientifically aligned with study data)
1) Eye10 – Heat 40°C / 20’
Gland decongestion according to Ocular Surface 2021.
Ophthalmogen Eye10 Advanced Eyecare
2) Ophthalmogen Gel — Biofilm/Demodex/Oil Cleansing
Necessary due to Clinical Dermatology 2021 (biofilm 28%).
Ophthalmogen Advanced Eyecare Gel
3) Ophthalmogen Spray — Hydration / Anti-Demodex / Redness Relief
Documented by Ocular Surface & AJO data.
FAQ – Συχνές Ερωτήσεις για το Έκζεμα & τη Δερματίτιδα Βλεφάρων
1. Τι είναι το έκζεμα βλεφάρων;
Το έκζεμα βλεφάρων είναι φλεγμονή στο λεπτό δέρμα γύρω από τα μάτια, με κοκκίνισμα, φαγούρα, ξηρότητα ή μικρές φουσκάλες. Μπορεί να οφείλεται σε ατοπική δερματίτιδα, σμηγματορροϊκή δερματίτιδα ή δερματίτιδα εξ επαφής.
2. What are the most common symptoms?
Κνησμός, κάψιμο, πρήξιμο, ερυθρότητα, λέπια/“πιτυρίδα” στις βλεφαρίδες, δακρύρροια, αίσθηση ξένου σώματος και συχνά βλεφαρίτιδα ή ξηροφθαλμία.
3. Ποιοι παράγοντες το προκαλούν ή το επιδεινώνουν;
Αλλεργιογόνα (καλλυντικά, βαφή μαλλιών, βερνίκι νυχιών), κολλύρια (αντιβιοτικά, αντιγλαυκωματικά), παράσιτα Demodex, βακτήρια, μύκητες (Malassezia), ξηρό κλίμα, άγχος και έντονο τρίψιμο των ματιών.
4. Είναι μεταδοτικό το έκζεμα βλεφάρων;
Όχι, το ίδιο το έκζεμα δεν είναι μεταδοτικό. Μπορεί όμως να συνυπάρχει με μολύνσεις (βακτηριακές, ιογενείς, Demodex) που χρειάζονται ειδική αντιμετώπιση από γιατρό.
5. Πώς σχετίζεται με τη βλεφαρίτιδα και την ξηροφθαλμία;
Η φλεγμονή των βλεφάρων επηρεάζει τους μεϊβομιανούς αδένες και το δακρυϊκό φιλμ. Αυτό οδηγεί σε Meibomian Gland Dysfunction (MGD), ξηροφθαλμία, θολή όραση και συχνά χαλάζια.
6. Πώς βοηθά η καθημερινή υγιεινή με Ophthalmogen;
Το σύστημα Ophthalmogen Eye10 – Gel – Spray αποσυμφορεί τους αδένες (Eye10), καθαρίζει απαλά λέπια, Demodex και biofilm (Gel) και καταπραΰνει/ενυδατώνει το periocular δέρμα με αντιφλεγμονώδη & αντι-Demodex δράση (Spray), μειώνοντας flare-ups.
7. Πόσο γρήγορα μπορώ να δω βελτίωση;
Συνήθως:
– 2–3 ημέρες → λιγότερο τσούξιμο/κάψιμο
– 1–2 εβδομάδες → λιγότερη ερυθρότητα & λέπια
– 3–4 εβδομάδες → καλύτερη λειτουργία αδένων και λιγότερα επεισόδια βλεφαρίτιδας, εφόσον τηρείται καθημερινό πρωτόκολλο.
8. Μπορώ να χρησιμοποιώ μακιγιάζ αν έχω έκζεμα βλεφάρων;
Ναι, αλλά προτιμώνται υποαλλεργικά προϊόντα, αποφυγή waterproof, ήπια αφαίρεση χωρίς τρίψιμο και πάντα καθαρισμός & ψεκασμός με Ophthalmogen μετά το μακιγιάζ.
9. Πότε πρέπει να πάω οπωσδήποτε σε οφθαλμίατρο/δερματολόγο;
Όταν υπάρχει έντονο πρήξιμο, πόνος, θολή όραση που δεν υποχωρεί, κίτρινες κρούστες, φυσαλίδες με υγρό, υποψία λοίμωξης ή όταν τα συμπτώματα δεν βελτιώνονται παρά τη σωστή υγιεινή.
10. Τι είναι η Δερμοφθαλμολογία και γιατί έχει σημασία;
Η Δερμοφθαλμολογία (Dermophthalmology) είναι η νέα επιστημονική ένωση Δερματολογίας & Οφθαλμολογίας που μελετά παθήσεις όπως έκζεμα, δερματίτιδα, ψωρίαση βλεφάρων και τη σχέση τους με το δακρυϊκό φιλμ.
Περισσότερα: Dermophthalmology.com & WOD.global






