What is ocular psoriasis?
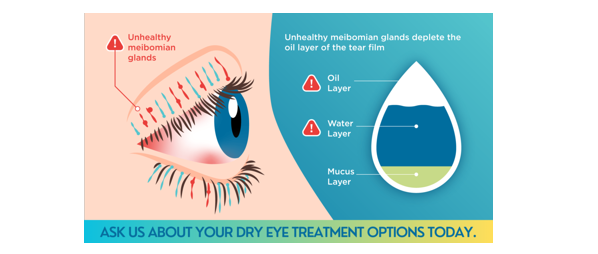
Ocular psoriasis is the involvement of psoriatic disease in the eyelids and ocular surface, causing inflammation, scaling, redness, dryness, and dysfunction of the Meibomian glands. It belongs to the field of Dermophthalmology (www.Dermophthalmology.com) and requires a combined dermatological and ophthalmological approach.
Psoriasis – Eyelids – Eyelashes – Eyes – Vision
Guidelines for a better quality of life for psoriasis sufferers
Psoriasis is a chronic autoimmune inflammatory disease that remains active for a long time, even for life in most patients.
It is estimated that 2-3% of the total population suffers from psoriasis, with 79% of patients believing that their lives have been negatively affected. 125 million people worldwide have psoriasis. The prevalence of psoriasis varies in different regions of the world, however, higher rates are reported in developed countries, corresponding to 4.6% of the population.
EYE DISCOMFORT AND BLURRED VISION ARE VERY COMMON IN PATIENTS WITH PSORIASIS
The health impact of psoriasis is not limited to the skin, but also affects many body systems including the eyes and vision. With the increasing literature on the association between psoriasis and extracutaneous systems, a better understanding of psoriasis as an autoimmune disease with systemic inflammation is emerging. In addition to cardio-metabolic diseases, gastrointestinal diseases, chronic kidney disease, malignancy and infections that have received attention, the association between psoriasis and more systemic diseases, including the cutaneous system, the ocular system, the reproductive system and the oral system, has also been revealed.
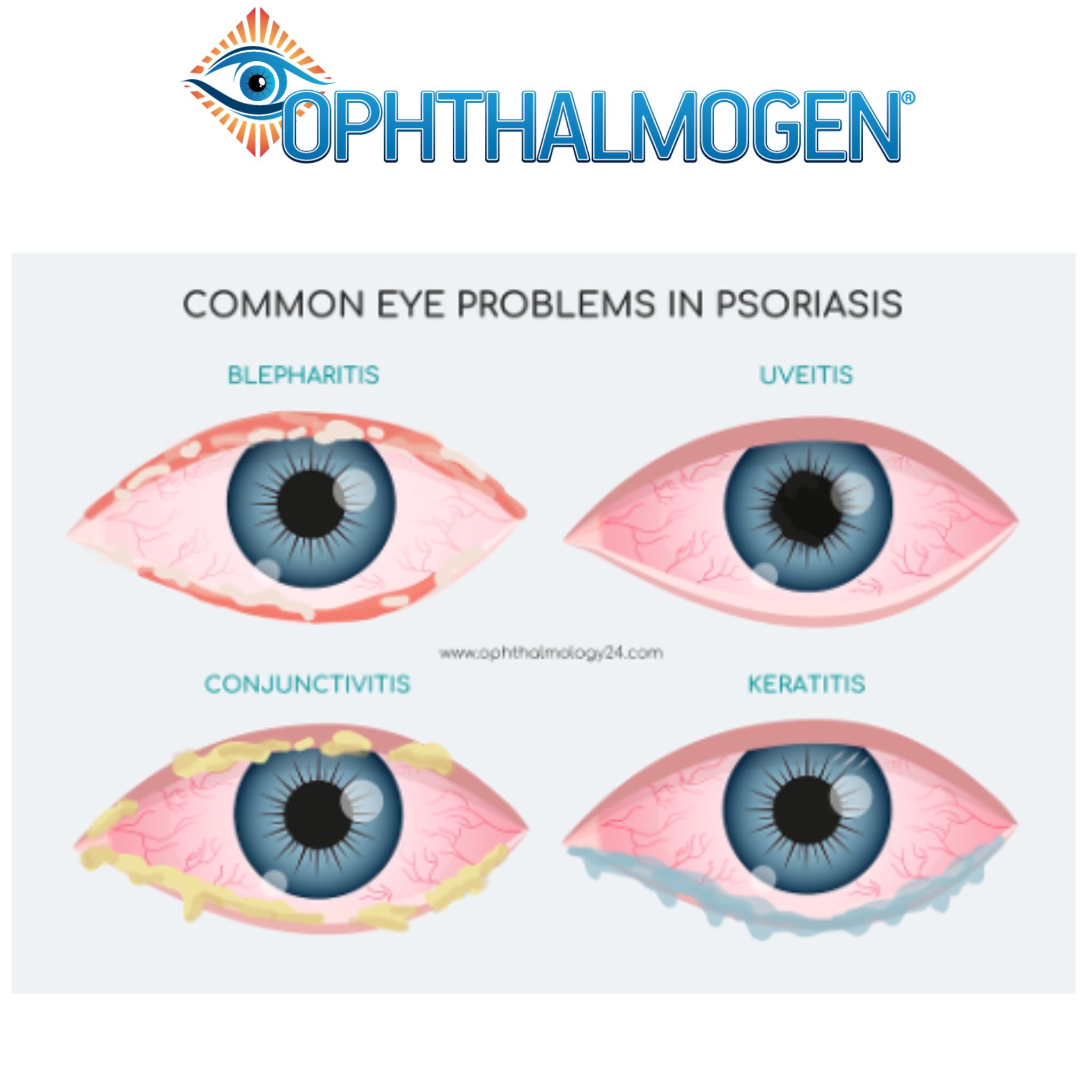
OCULAR PSORIASIS AFFECTS ALL PARTS OF THE EYE
Ocular psoriasis can involve any structure of the eye, including the eyelid, conjunctiva, lacrimal gland, and uvea.
BLEPHARITIS IS THE MOST COMMON DISEASE IN PATIENTS WITH PSORIASIS
Blepharitis has been found to be the most common ocular disease in patients with psoriasis. Corneal involvement in psoriasis is rare and probably secondary to eyelid or conjunctival complications, such as dry eye and trichiasis. Dry eye and trichiasis can lead to erosions of the corneal epithelium.
As ocular complications of psoriasis are very common, they can affect almost any part of the eye. Blepharitis/dry eye, madarosis, trichiasis, and ectropion are the most common ocular manifestations associated with psoriasis.
CONJUNCTITIS IS A VERY COMMON COMORBITION OF PSORIASIS
UP TO 65% OF PATIENTS WITH PSORIASIS MAY BE AFFECTED BY CONJUNCTITIS
Another particularly common pathogenesis of psoriasis patients is conjunctivitis, which can affect up to 65% of patients. Chronic nonspecific conjunctivitis is the most common form of conjunctivitis among psoriasis patients. Psoriasis can affect almost any structure of the eye. However, the most common manifestations include blepharitis, dry eyes, and conjunctivitis. Depending on the area involved and the severity of the conditions, the signs and symptoms of ocular psoriasis can vary from asymptomatic erythema to debilitating scarring and vision loss.

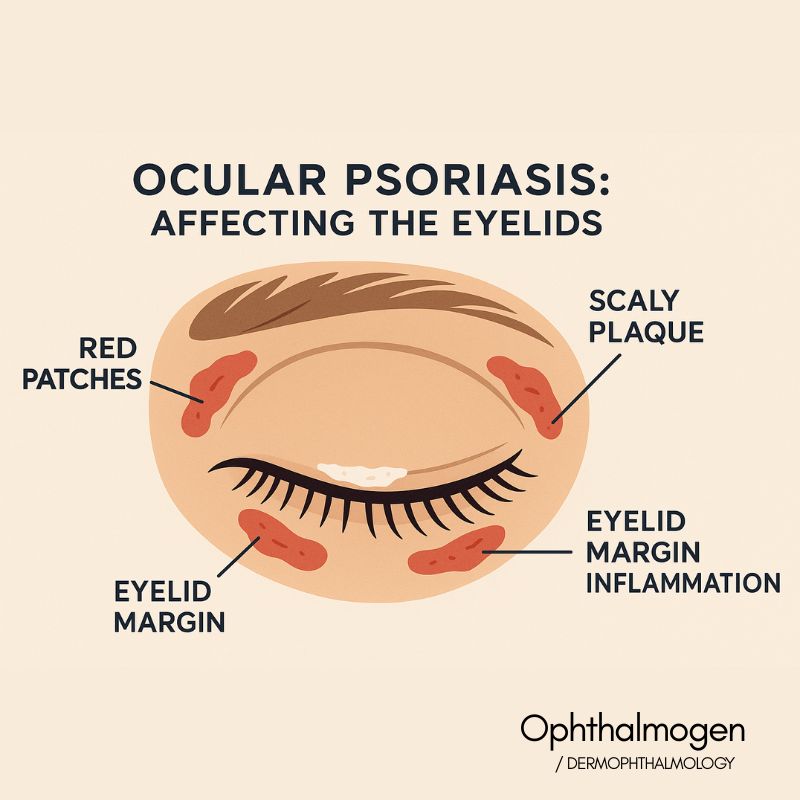
EYELID PSORIASIS
67-67.4% of patients with psoriasis have ocular manifestations mainly in the anterior segment of the eye that may reduce the quality of vision, the appearance of the eyes and their quality of life. It is commonly accepted based on multiple scientific data that blepharitis, dry eyes and conjunctival hyperemia (red eyes) are very common ocular effects. Changes in the tear film, the surface of the conjunctiva, impaired function of the meibomian glands and overpopulation of Demodex parasites are particularly common pathological conditions among patients with psoriasis.
IGNORANCE OF EYELID HYGIENE DETERMINES QUALITY OF LIFE
Because the majority of psoriasis patients do not know the importance of eyelid hygiene, they will have most of the symptoms due to uncontrolled inflammation from Demodex & bacteria which multiply rapidly in the absence of hygiene. If you have not learned to take care of your eyelids from a young age, then the likelihood of suffering from your eyes is very high. Massaging, spraying and decongesting the eyelids, as well as resting the eyes with products Ophthalmogen Protocol It is considered the cornerstone of good eye health and vision.
CATARACTS & UVEIDITIS: PSORIASIS COMMON COMPLICATIONS
Several important scientific studies have reported in the past that patients with psoriasis may develop cataracts, while another important scientific fact is that 7-25% of patients with psoriasis may develop uveitis, a very serious eye disease.
It is also scientifically proven that scalp psoriasis is significantly associated with blepharitis/dry eyes.
THE PARASITES DEMODEX IT IS ONE OF THE MAIN CAUSES OF BLEPHARITIS & DRY EYES
Based on scientific data, 18% of psoriasis patients have dry eyes, while 30-45% of cases of dyskeratosis can affect the eyelids with blepharitis, ectropion, entropion, trichiasis, alopecia areata, pterygium, nasolacrimal duct obstruction with epiphora, and conjunctivitis.
DERMATO-OPHTHALMOLOGICAL PROBLEMS ARE PARTICULARLY FREQUENT IN PATIENTS WITH PSORIASIS
The impact of skin diseased with pathological keratinization processes on eye function and vision is often underestimated by clinicians, which can have dramatic consequences for the patient, including vision loss due to changes in the ocular surface (corneal ulcers and perforations), fundoscopic manifestations (retinal neovascularization, retinal angiopathy, optic nerve atrophy)

AMERICAN ACADEMY OF OPHTHALMOLOGY
PSORIASIS IS NOT LIMITED TO THE SKIN AND OFTEN AFFECTS THE EYES
According to the American Academy of Ophthalmology, the most common form of psoriasis is plaque psoriasis, which accounts for 80% of all psoriasis cases. Ocular manifestations of psoriasis include blepharitis, conjunctivitis, uveitis, episcleritis, and cataracts. Psoriasis is not limited to the skin and can affect other organs, including the cornea and lacrimal gland, which can lead to dry eyes.
Meibomian gland dysfunction is more prevalent in patients with psoriasis. Patients may experience signs of sensitivity to light.
UVEIDITIS – A SERIOUS EFFECT OF PSORIASIS
The mechanism between uveitis and psoriasis remains complex and multifactorial, but the two disorders have been found to share common immunological pathways. The incidence of uveitis in psoriasis is estimated to be 7-20% with severe and mild cases of psoriasis at increased risk. Patients may present with signs of light sensitivity, blurred vision, and sometimes floaters in the visual field.
STATISTICS OF THE OCCURRENCE OF EYE SYMPTOMS IN PSORIASIS
- 75% of patients with plaque psoriasis have ocular manifestations
- 50-60% of patients with psoriasis have ocular manifestations. Ocular manifestations are most commonly seen in patients over 51 years of age.
- 85% of psoriasis patients receiving systemic treatment in the form of methotrexate tablet along with topical steroids have ocular manifestations
- 79% of patients with scalp psoriasis have ocular manifestations
- 87.07% of patients with common psoriasis have ocular manifestations
THE OVERALL MANAGEMENT OF OCULAR MANIFESTATIONS OF PSORIASIS OFTEN REQUIRES A MULTIPROFILE APPROACH THAT INCLUDES DERMATOLOGISTS & OPHTHALMOLOGISTS AT THE CENTER
Dermatologists, ophthalmologists, and rheumatologists should be vigilant when examining patients with psoriasis, and a multidisciplinary approach should be implemented for the early diagnosis of ocular psoriasis to manage unnecessary ocular discomfort, reduce quality of life, minimize eye damage, and prevent possible permanent vision loss. Ocular manifestations of psoriasis may be subtle and missed in the absence of regular ophthalmological examination.
HOW IS PSORIASIS ON THE EYELIDS-EYELIDS-EYES TREATED?
- Make use of Ophthalmogen Eye10 self-heating masks at a constant temperature of 40C for 20 minutes. Daily use for severe symptoms and occasional use for moderate symptoms will significantly improve all parameters of local inflammation and at the same time the quality of your vision.
- Spray the eyelids and the eye area daily with Ophthalmogen Spray (you let it dry and don't rinse it off).
- Wash your eyelids daily with Naviblef Daily Care foam. For severe symptoms and flare-ups, use Naviblef Intensive Care for 15 days every three months.
- Incorporate daily eyelid massage with it from the very first moment. Ophthalmogen Gel (ointment also for Demodex blepharitis). This way you will keep the inflammation in the eyes under control as well as the number of Demodex parasites/bacteria. The relief of the whole range of annoying eye symptoms that bother you will be long-lasting. Due to the natural composition of the gel Ophthalmogen Protocol you can use it daily.
- In some cases, you will be advised to use topical medications such as corticosteroid creams (cortisone) or tacrolimus ointment on your eyelids, but for a short period of time. Your chronic main treatment remains the use of self-heating masks. Ophthalmogen Eye10, spraying with Ophthalmogen Spray, eyelid cleaning and massage Ophthalmogen Gel (
steps 1, 2, 3, 4) - The use of antibiotics will be recommended in the event of a skin infection.
- Artificial tears in the form of drops such as Visionlux Plus Duo and in spray form such as Flora Vision are ideal for psoriasis patients. Instill and spray directly onto the ocular surface, with eyes open.
The scientific understanding of ocular psoriasis is part of the WOD-World Organization of Dermophthalmology (www.WOD.
Questions - Answers
1. What is ocular psoriasis?
Ocular psoriasis is the involvement of psoriatic disease in the eyelids and ocular surface, causing inflammation, scaling, redness, dryness, and dysfunction of the meibomian glands.
2. What are the most common symptoms?
redness of the eyelids
scales or plaques
τράβηγμα/σφίξιμο στο βλέφαρο
dry eye symptoms
excessive lacrimation
irritation or a "sandy" feeling
3. Where exactly does psoriasis appear on the eyes?
It usually appears:
on the upper eyelid
on the lower eyelid
in the lid margin area
on the eyebrows
peri-ocular
4. Can ocular psoriasis cause blurred vision?
Yes, when there is inflammation of the ocular surface or severe meibomian gland dysfunction (MGD), it can cause temporary blurred vision.
5. Is it contagious?
No. Psoriasis is not contagious.
6. How is the diagnosis made?
The diagnosis is made by an ophthalmologist and dermatologist, with a clinical examination of the eyelids and the skin around the eyes.
7. What is the relationship with Dermophthalmology;
Ocular psoriasis belongs to the field of Dermophthalmology, the science that unites Dermatology and Ophthalmology for eyelid and ocular surface diseases.
8. What is the treatment?
Treatment includes:
daily eyelid hygiene
hydration
inflammation regulation
treating MGD
special products for eyelids
(e.g. Ophthalmogen Gel, Ophthalmogen Spray, Eye10 θερμοκομπρέσα)
9. Can it relapse?
Yes. Psoriasis is a chronic condition with periods of flare-ups and remissions.
10. When should I seek medical help?
when there is a sudden deterioration
persistent blurred vision
severe pain
swelling or discharge
deterioration of eyelashes