Introduction
Watery eyes are among the most common yet underestimated complaints in eye care. Thousands of people live with constant tearing, carrying tissues, with red eyelids and a heavy sensation — and consider it “normal.”
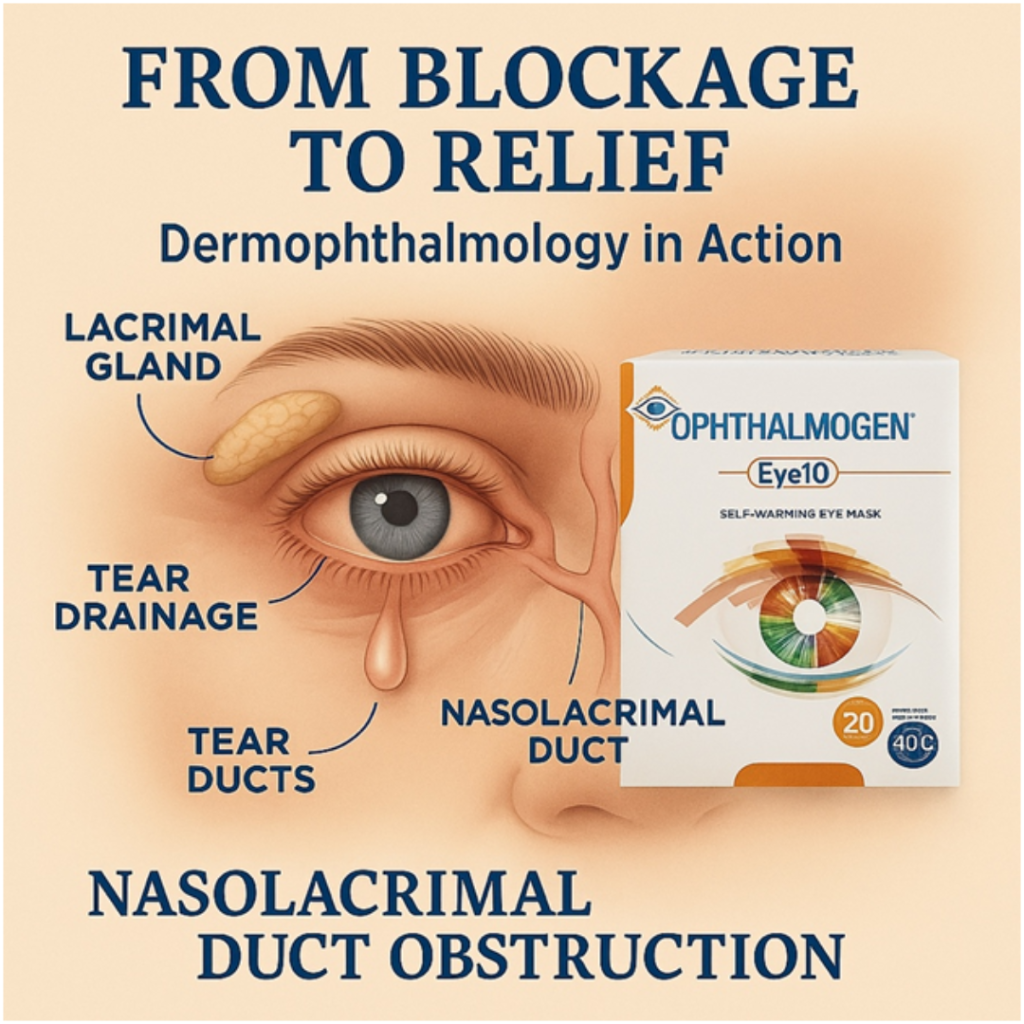
In reality, the leading cause is nasolacrimal duct dysfunction or obstruction, which prevents tears from draining properly into the nose.
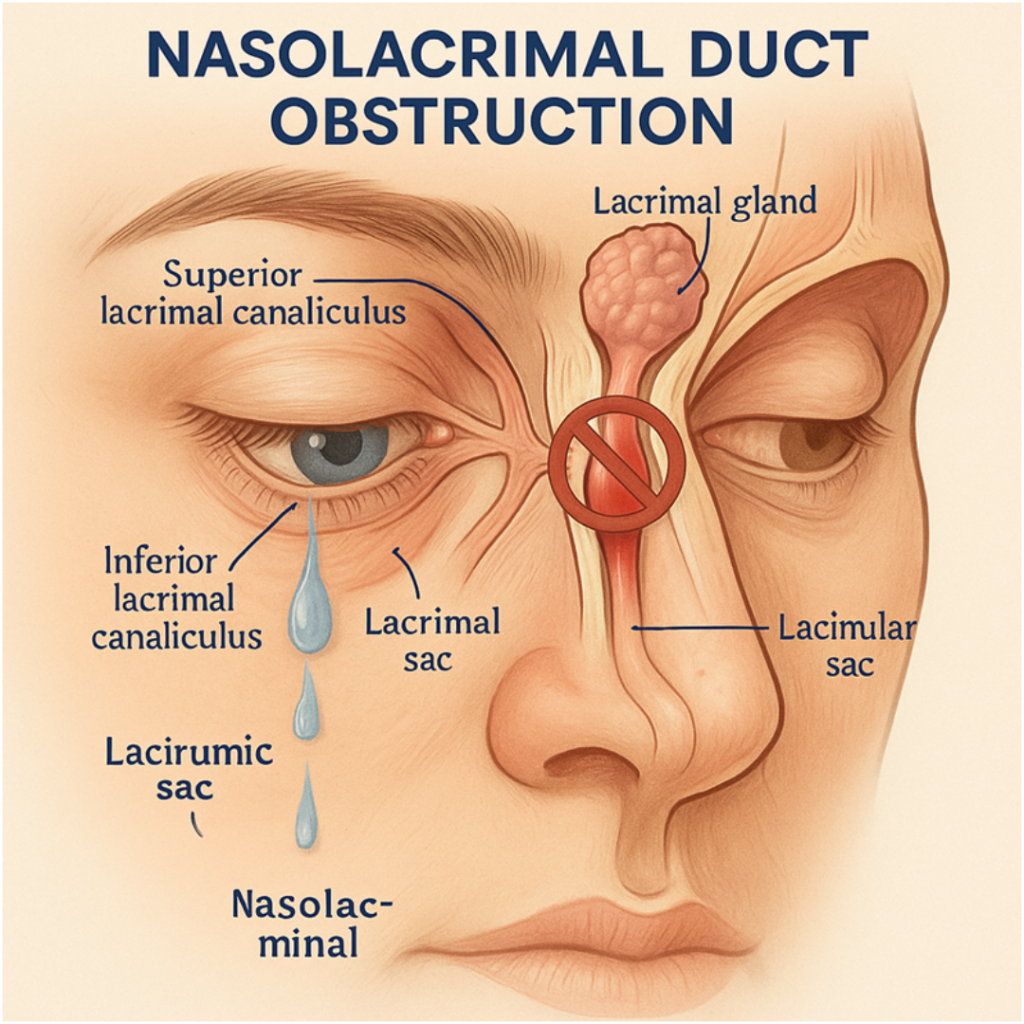
Anatomy & Physiology of the Lacrimal System
- The nasolacrimal duct is a narrow tube, ~12–18 mm in length and ~2 mm in diameter, connecting the lacrimal sac to the nasal cavity.
- Its diameter is small (~2 mm), which makes it vulnerable to inflammation and stenosis.
- The lacrimal sac functions as a "reservoir" that stores and promotes tears.
- Every time we blink, the eyelid pump helps tears pass into the duct.
When the pump (eyelid) malfunctions or the duct narrows, lacrimation occurs without crying.
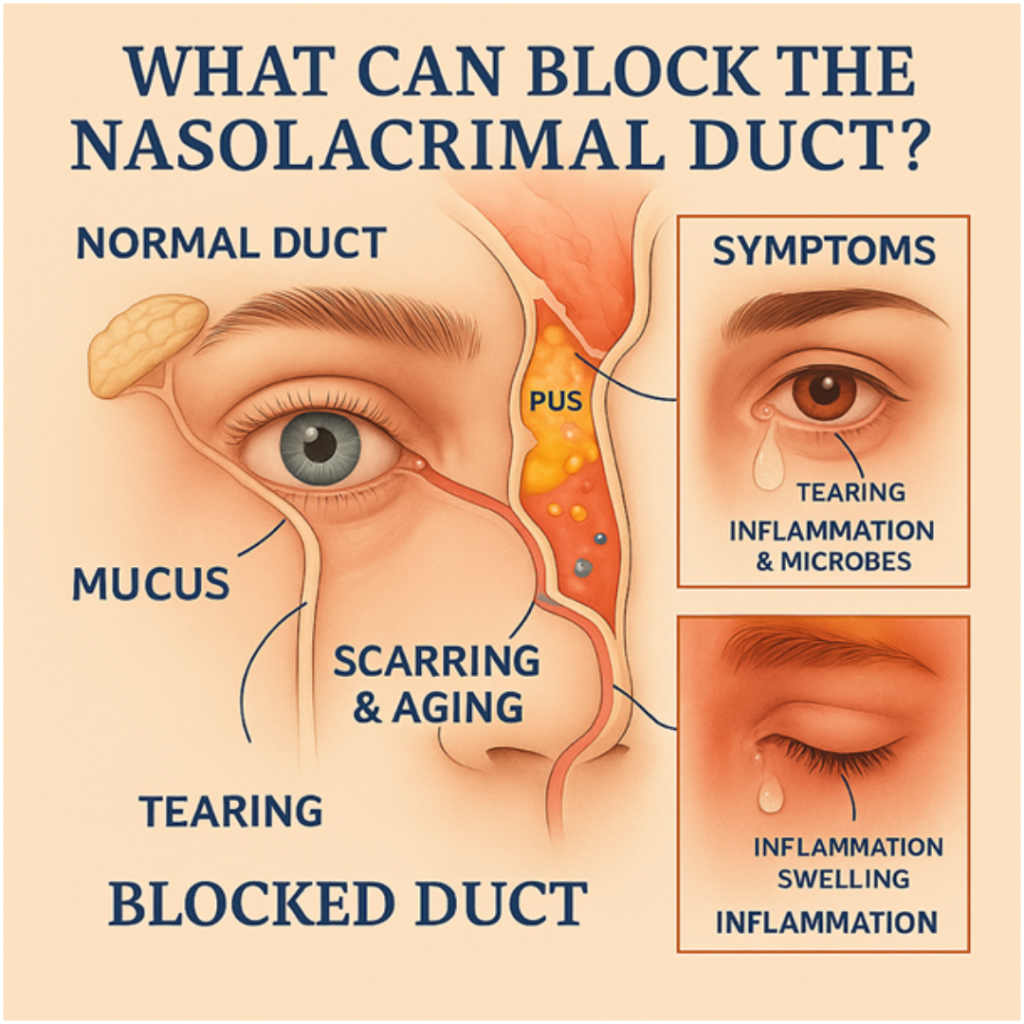
Causes of Nasolacrimal Duct Blockage
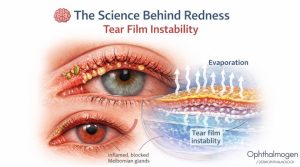
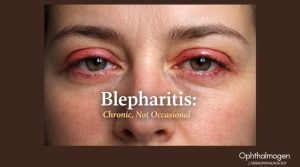
- Inflammation & edema (allergic rhinitis, chronic blepharitis, dry eye).
- Mucus & cellular debris in the lacrimal sac.
- Fibrosis & scarring from chronic inflammation or trauma.
- Congenital stenosis in newborns.

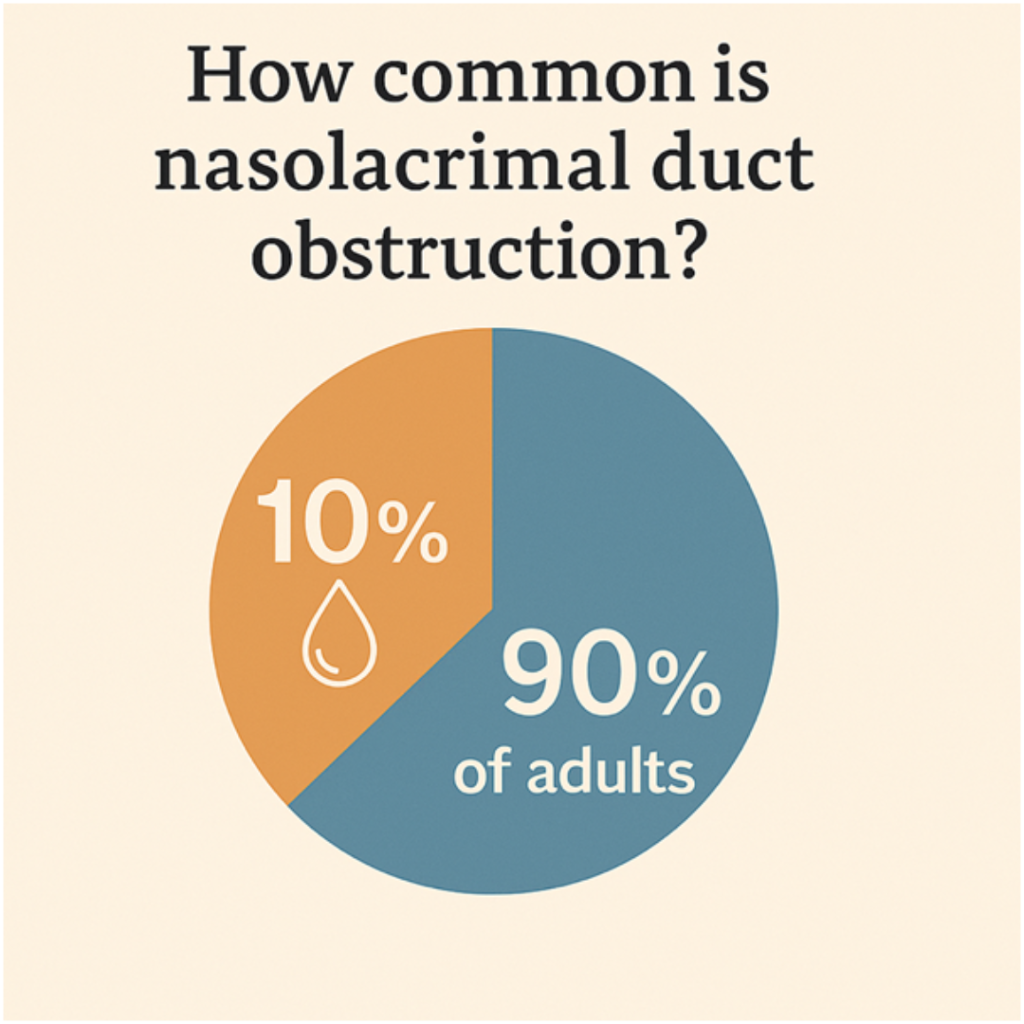
How Common Is the Problem?
- Infants: Congenital obstruction affects 5–10% of newborns; in 90% it resolves spontaneously within the first year with massage & compresses.
- Adults (40–70 years): Officially 3–6%, but likely closer to 8–12%, as many simply live with tearing undiagnosed.
- Elderly (70+):>10%.
- Women: Higher prevalence due to hormonal changes and narrower ducts.
Causes of Nasolacrimal Duct Blockage
- In Asia, prevalence may reach 15% due to anatomical differences.
- In Europe & the US, reported rates are lower, but underestimation is significant due to poor diagnostic awareness.

- Hippocrates & Galen described “tear-related diseases.”
- 19th century: first surgical techniques for dacryocystorhinostomy (DCR).
- 20th century: endonasal & endoscopic approaches improved outcomes.
- Yet, the cornerstone of prevention — daily eyelid hygiene & nasal care — remains underutilized.
The Social Dimension

Chronic tearing:
- Disrupts work and productivity.
- Creates the impression of “sick eyes.”
- Raises costs (eyedrops, visits, surgery, lost productivity).
Eye hygiene is not a luxury but a cost-effective form of prevention.
Links With Other Conditions
- Glaucoma: Antiglaucoma drops induce chronic surface inflammation → tearing & blepharitis.
- Allergic rhinitis: Nasal congestion increases pressure on the duct → tearing & dark circles.
- Dry eye & blepharitis: Inflammation near the puncta can trigger obstruction.
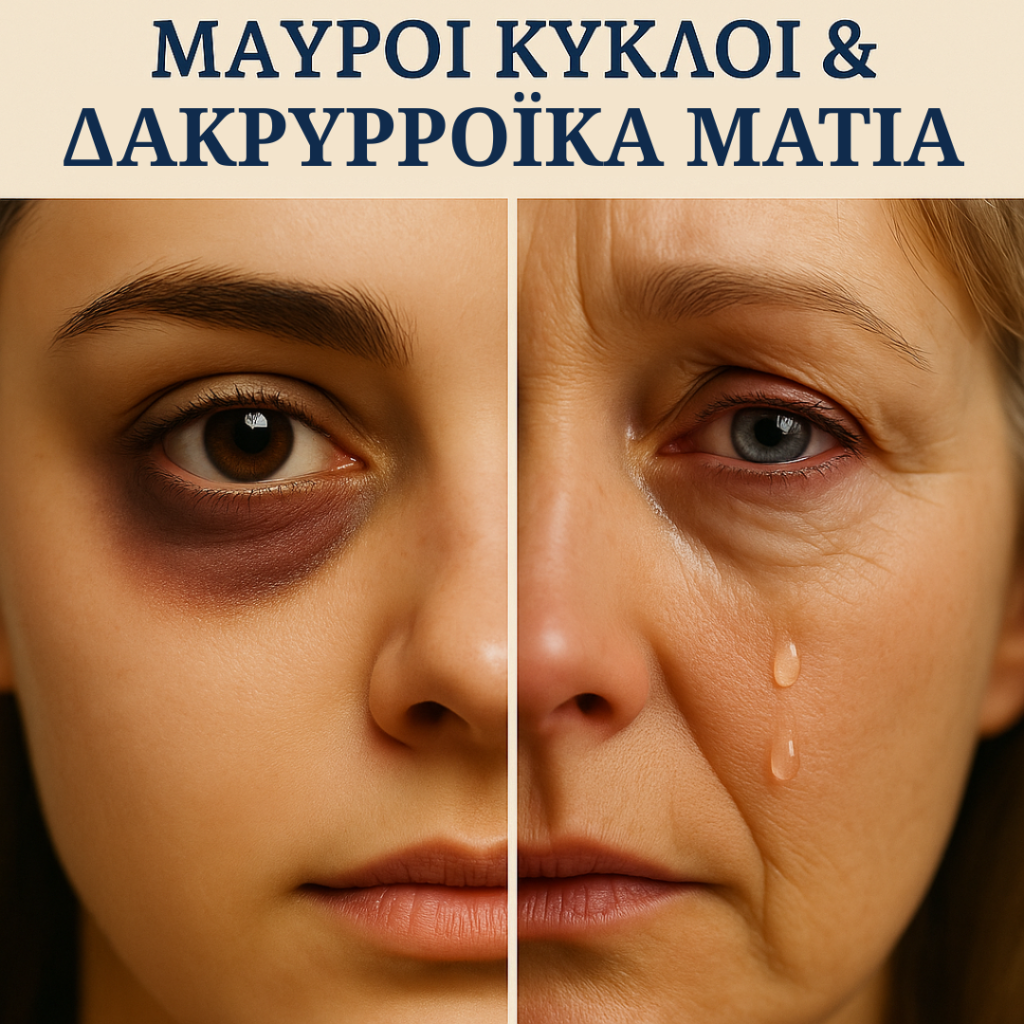
Dark Circles & Watery Eyes
Chronic congestion around the lacrimal drainage system:
- Impairs microcirculation.
- Creates shadows under the eyes (dark circles).
- Links watery eyes not only to a medical but also an aesthetic burden.
Thus, blockage is not only a medical but also an aesthetic problem.

Self-Care Protocol
Step 1 – Thermal Therapy (EYE10)
40°C for 15–20 minutes, once or twice daily.
Goal: tissue relaxation, improved flow.
Step 2 – Lacrimal Sac Massage
After thermal therapy, downward pressure at the inner canthus (5–10 times)with Ophthalmogen Gel massage.
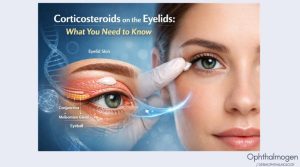
Step 3 – Eyelid Hygiene
- Naviblef Daily Care (or Intensive).
- Ophthalmogen Spray for microbial &Demodex control.
Step 4 – Tear Film Stabilization
- Visionlux Plus / Flora Vision Spray.
Βήμα 5 – Ρινική Υποστήριξη
- OTOSAN Nasal Spray Forte.
- OTOSAN Baby.
- OTOSAN Nasal Wash with hyaluronic acid.

Case Studies
- Infant, 5 months: Congenital obstruction → resolved with massage.
- Woman, 47, allergic rhinitis: Self-Care Protocol → marked improvement, no surgery needed.
- Man, 72, chronic blepharitis: Limited improvement → underwent DCR → full resolution.
Future Studies
- Real epidemiology (true prevalence likely >10%).
- Effectiveness of a 6-week Self-Care Protocol (EYE10 + Naviblef/Ophthalmogen + OTOSAN).
- Ophthalmology–ENT comparative studies on DCR.
- Cost-effectiveness of conservative vs surgical care.
FAQ
- Why are my eyes watering if I’m not crying?
Because tears cannot drain due to narrowing or inflammation of the duct.
- Can I manage it at home?
Yes: OphthalmogenEYE10 compresses, massage with Ophthalmogen Gel, Naviblef eyelid cleansing, OTOSAN NASAL WASH with hyaluronic cleansing & hydration of the nasal mucosa .
- When is surgery required?
For complete or resistant obstruction.
- Who performs the surgery?
Oculoplastic ophthalmologists or ENT surgeons, usually in collaboration.

Conclusion & Collaboration Bridge
Nasolacrimal duct obstruction is underdiagnosed, not rare.
Daily hygiene and nasal support are key, not surgery alone.
Important Note:
Dermophthalmology does not replace Ophthalmology; it complements it. Self-Care protocols reduce inflammation and improve patients’ daily lives, so they reach the doctor better prepared. When conservative care is insufficient, collaboration with Ophthalmologists and ENT specialists is essential. The shared goal: health, relief, and quality of life.
Dermophthalmology is the new medical specialty we have introduced (learn more at www.dermophthalmology.com)