The New Interpretation of Presbyopia
For centuries, presbyopia — the gradual loss of near focus after the age of forty — was considered a natural consequence of aging, an unavoidable hardening of the lens. However, 21st-century science reveals a deeper reality: presbyopia is not merely mechanical sclerosis but a systemic imbalance — involving low-grade inflammation, dehydration, and reduced microcirculation.
Dermophthalmology, the new discipline bridging the eye and the skin, marks a turning point in ophthalmic medicine. Vision is no longer seen as a purely mechanical act, but as a biological and energetic equilibrium — the harmonious interaction of light, tissue, circulation, and care.
From Aristotle to Helmholtz – The Chronicle of a Vision
The quest to understand vision began in ancient Greece. Aristotle (384–322 BC) described sight as a “fusion of light and matter,” recognizing the need for a clear medium — a concept that foreshadowed today’s understanding of the tear film.
Centuries later, Galen (2nd century AD) proposed that vision results from a “spiritual flow of light” (spiritus visibilis) emanating from the brain toward the eyes, an early precursor to today’s neuro-optical model of visual function.
In 1666, Heinrich Meibom discovered the Meibomian glands, establishing the basis for eyelid physiology.
Almost two centuries later, Hermann von Helmholtz (1821–1894), a physician, physiologist, and physicist, presented his groundbreaking Accommodation Theory (1855), which defined the classical view of presbyopia for the next 150 years.
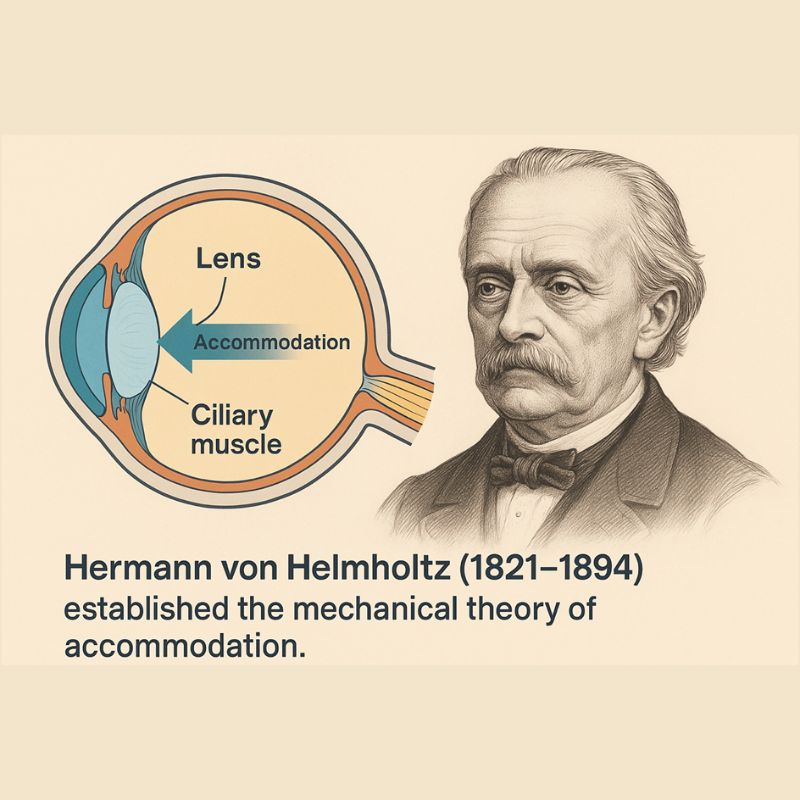
Helmholtz and His Era
Helmholtz lived in 19th-century Germany — an age deeply shaped by Newtonian mechanics, where all biological processes were explained as mechanical reactions.
In 1855, he proposed that accommodation is achieved through changes in the shape of the lens caused by contraction or relaxation of the ciliary muscle. When we focus near, the ciliary muscle contracts and the lens becomes more convex; when we focus far, the muscle relaxes and the lens flattens.
It was an extremely intelligent and groundbreaking interpretation for its time. But Helmholtz based his theory on observations of cadavers and isolated eyes, not on living tissue. There were no microscopes at the time, nor any way to observe ocular function in vivo.
Microbiology, Embryology, and Neurophysiology had not yet been born; the concept of systemic inflammation or skin-eye interaction was unthinkable. In this context, the mechanical explanation of the lens was revolutionary—but necessarily incomplete.
Helmholtz’s model ignored factors that we now know critically affect accommodation:
– the role of the tear film,
– neurovascular regulation,
– low-grade inflammation,
– and the function of the Meibomian glands.
The Challenge to the Mechanical Model
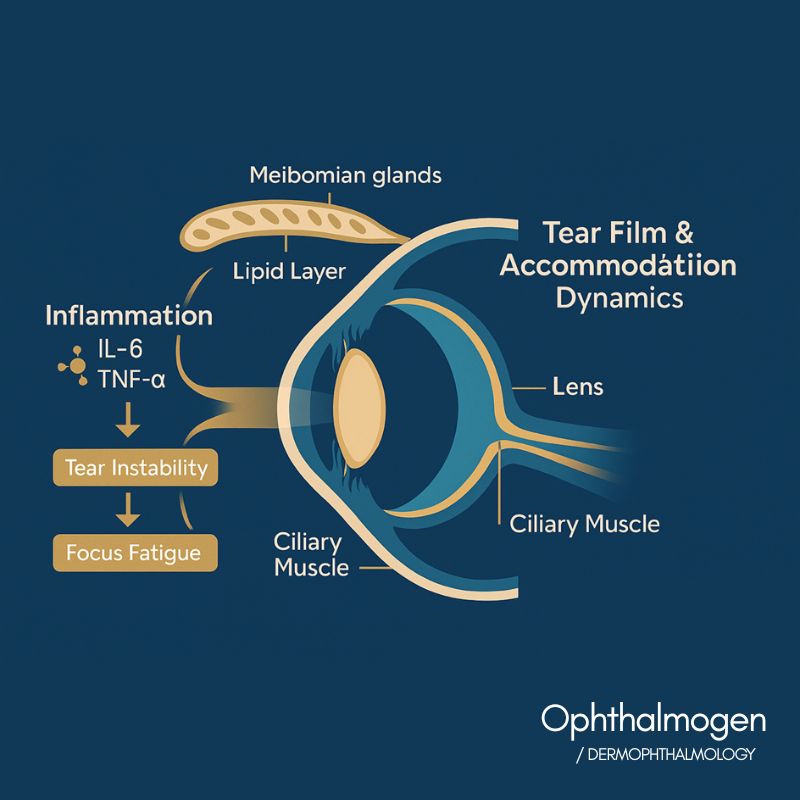
Since the 1990s, advances in wavefront aberrometry, confocal microscopy, and tear interferometry have revealed that accommodation loss cannot be explained by lens elasticity alone.
Glasser & Campbell, Vision Research, 1998: Lens elasticity declines with age, but ciliary muscle contractility remains functional even in older adults.
Croft et al., Exp Eye Res, 2006: Accommodation loss correlates with ocular surface inflammation and reduced microvascular perfusion.
Craig et al., Ophthalmic Physiol Opt, 2021: Fluctuations in tear film stability cause micro-variations in accommodation and near-vision fatigue.
Yoshida et al., J Cataract Refract Surg, 2020: Mild Meibomian gland dysfunction impairs near-vision quality even before optical changes appear.
These findings established presbyopia as a multifactorial condition — where inflammation, dehydration, tear-film instability, and vascular decline act together.
The Dermophthalmologic Interpretation


The Practical Revolution – Ophthalmogen
Medicine returns to its Greek roots.
Hippocrates taught that “the body heals when its balance is restored.” Hygieia, daughter of Asclepius, symbolized purity and prevention. Dermo-Ophthalmology continues this tradition: purity is healing; light is prevention.
Article Significance
This article brings together four sciences—Ophthalmology, Dermatology, Neurobiology, and Microcirculation—and redefines presbyopia as an indicator of inflammatory balance, not aging.
It highlights Dermo-Ophthalmology as the bridge between science and the philosophy of health, and positions daily eyelid care as the new act of medical prevention.
Bibliographic References
- Helmholtz H. Handbuch der Physiologischen Optik, 1855.
- Glasser A, Campbell MC. Vision Research, 1998.
- Croft MA et al. Exp Eye Res, 2006.
- Yoshida M et al. J Cataract Refract Surg, 2020.
- Craig JP et al. Ophthalmic Physiol Opt, 2021.
- Millar TJ et al. Prog Retin Eye Res, 2023.
- Wang Y et al. Front Neurosci, 2019.
- Papadopoulos A et al. Hellenic Ophthalmic Rev, 2024.
In Summary
From Meibom to Helmholtz and from Craig to Dermo-Ophthalmology, the science of vision traces a 350-year historical trajectory. Presbyopia is not the end of youthful vision — it is an invitation to restore balance. Cleanliness, warmth and care of the eyelids are the new medical practice of prevention.
Discover the full Ophthalmogen range at www.ophthalmogen.com and Dermophthalmology at www.Dermophthalmology.com
Give your eyes the care and beauty they deserve.