How it affects the ocular surface, the gaze, and vision | Dermophthalmology Edition |
Eczema (eczema / dermatitis) is one of the most common inflammatory skin conditions, but when it affects the eyelids it gains much greater clinical importance. The eyelid skin is 4 times thinner than the facial skin, which makes it more vulnerable to:
- inflammation
- allergens & cosmetics
- microbes & Demodex
- irritant substances
- topical or ocular medications
- environmental factors
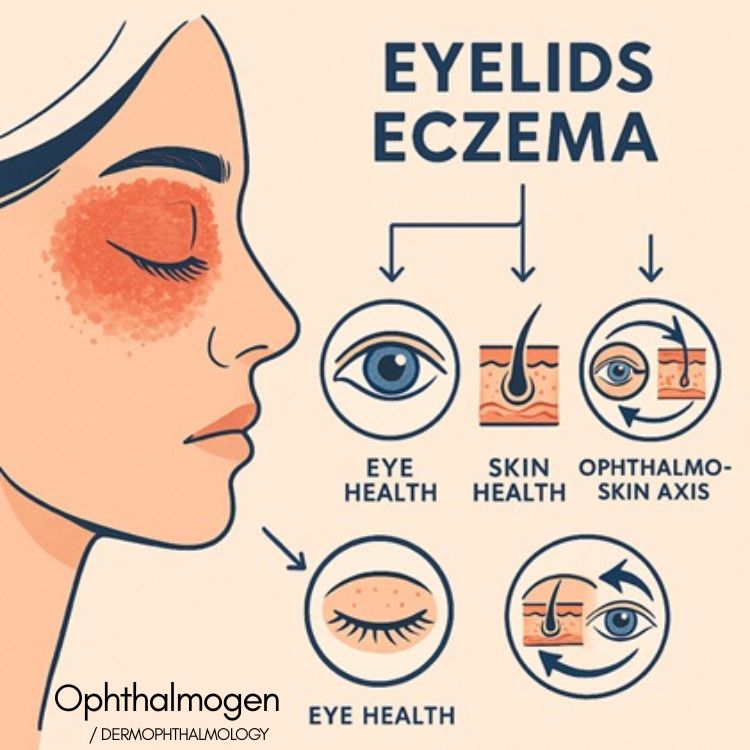
According to international studies, eyelid eczema is one of the skin disorders that most directly affects:
(Dermophthalmology Method Insight The new perspective on eczema
Η Δερμοφθαλμολογία (Dermophthalmology) είναι το νέο επιστημονικό πεδίο που ενώνει:
- Dermatology:
- Ophthalmology:
- The Ophthalmo-Skin Axis (skin–eyelid–tear-film system)
Within this framework, eyelid eczema is no longer viewed as a “purely skin problem,” but as a dermato-ocular condition that:, αλλά:
- directly affects the eyelid barrier
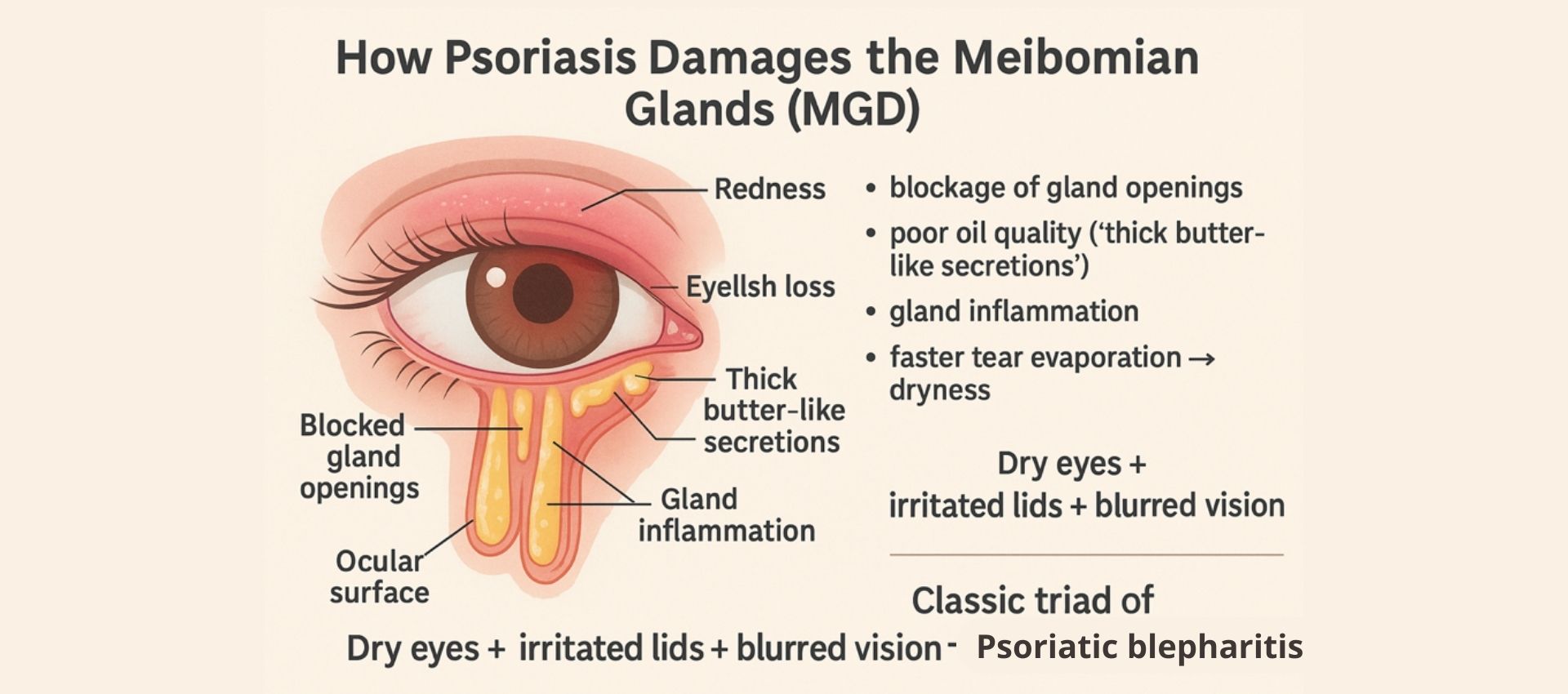
- disrupts Meibomian gland function
- destabilizes the tear film
- leads to blepharitis, dry eye, blurry vision, chalazia
- What is eczema on the eyelids?
Eyelid eczema can present as:
- atopic dermatitis
- seborrheic dermatitis
- contact dermatitis (allergic / irritant)
- periocular dermatitis
- blepharodermatitis
Main symptoms include:
- redness, irritation, itching
- dryness, scaling, crusting
- burning sensation & swelling
- sensitivity at the eyelid corners
- recurrent blepharitis, chalazia
- tearing or blurry vision
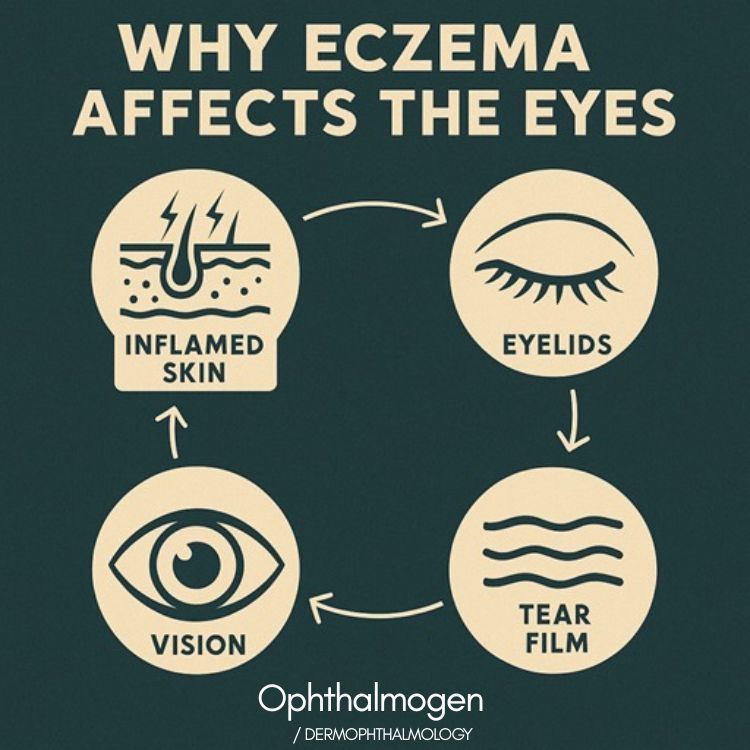
2. Why does eczema affect the eyes so much?
The Dermophthalmology explanation – Ophthalmo-Skin Axis
Dermophthalmology describes the skin, eyelids, and tear film as one functional unit — the Ophthalmo-Skin Axis.
Why?
•they share a common embryological origin (ectoderm)
•the periocular skin is directly linked to the Meibomian glands
•skin inflammation → spreads to the eyelids → alters the tear film
•eyelids regulate the tear film and thus vision
So eczema is not only a skin disease; it is also an ocular disease.
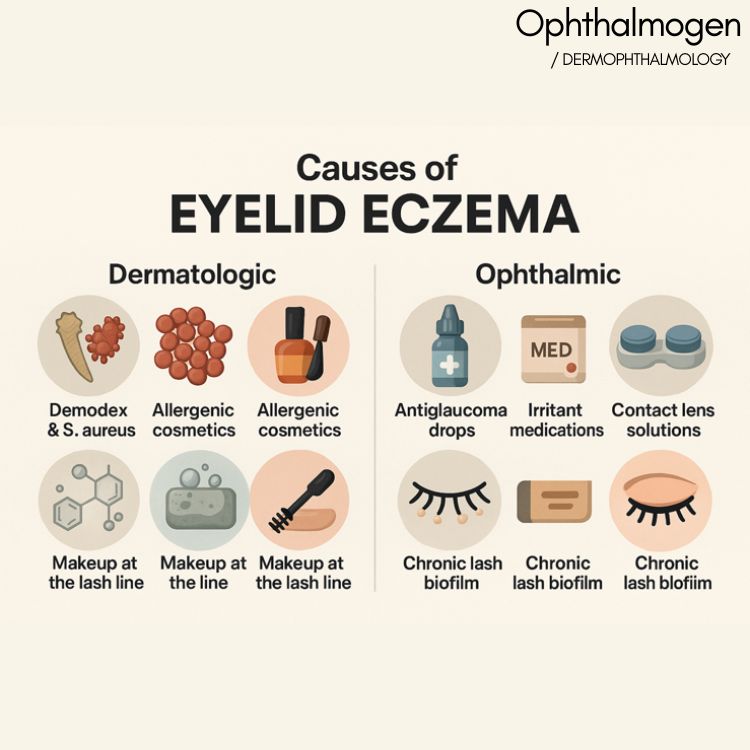
3. What causes eczema on the eyelids?
Skin-related causes
• Demodex & Staphylococcus aureus
•impaired skin barrier
•allergenic cosmetics
•soaps, chemicals, detergents
•nail polish / nail products (secondary transfer to eyelids)
•pollutants & makeup along the lash line
Related article (makeup & blepharitis):
Eye-related causes
•anti-glaucoma eye drops
•topical medications causing irritant dermatitis
•contact lens solutions and preservatives
•chronic biofilm on the eyelashes
4. Link between eczema and eye diseases
Eczematous skin disrupts eyelid and tear-film function, leading to:
•Blepharitis: The most common complication. Related to Demodex, microbes, and blocked Meibomian glands.
Full Dermophthalmology article
•Dry Eye (Evaporative dry eye): Inflammation impairs Meibomian gland function → poor-quality lipids → increased tear evaporation. Related article:
• Blurred vision: Due to tear-film instability and surface irregularities.:
• ConjunctivitisVery common in atopic patients (allergic and irritant conjunctivitis).
• Chalazion: Because of blocked Meibomian glands in a chronic inflammatory environment.
• Tearing (epiphora): Paradoxical sign of evaporative dry eye:
• Red eyesDue to acute or chronic inflammation of the ocular surface. Full Article
5. What does science say? – 7 Key Studies
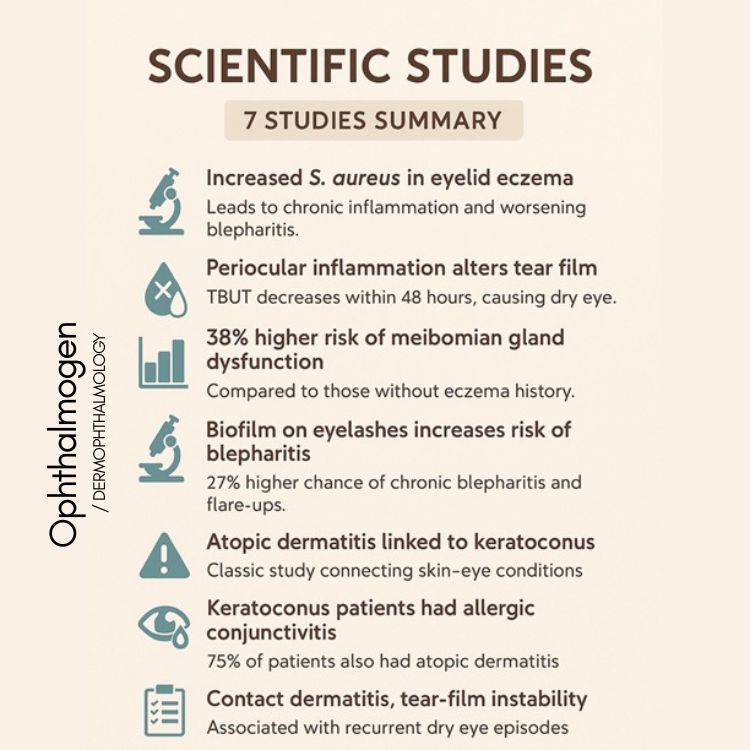
• Study 1 — Journal of Dermatology, 2018
Eyelid eczema is associated with increased Staphylococcus aureus on the lashes and periocular skin, leading to chronic inflammation and worsening blepharitis.
Study 2 — The Ocular Surface, 2021
Periocular skin inflammation can alter tear breakup time (TBUT) within 48 hours, resulting in dry eye symptoms.
• Study 3 — Cornea Journal, 2019
Patients with eczema have a 38% higher likelihood of developing Meibomian Gland Dysfunction (MGD) compared with non-eczematous controls.
• Study 4 — Eye & Contact Lens, 2020
Biofilm on the eyelashes increases the risk of chronic blepharitis by 27% and contributes to recurrent flare-ups.
• Study 5 — British Journal of Ophthalmology, 1977 (Hilgartner)
A classic paper showing that atopic dermatitis is associated with an increased risk of keratoconus.
• Study 6 — ARVO, 2024 (Annual Meeting)
75% of patients with keratoconus also had allergic conjunctivitis and atopic dermatitis, confirming the skin–eye link.
• Study 7 — Clinical Ophthalmology, 2022
Eyelid contact dermatitis is strongly associated with tear-film instability and recurrent dry eye episodes.
6. How is the diagnosis made?
Dermatologists and ophthalmologists typically assess:
• lash line
•eyelid skin (redness, scaling, swelling)
•presence of Demodex (lashes, blepharodermatitis)
•Meibomian gland function
•the tear film (TBUT, lipid quality, staining)
•periocular skin (erythema, edema, texture)
They must rule out:
•psoriasis
•rosacea
•infectious eczema
•allergic dermatitis
•periocular rosacea
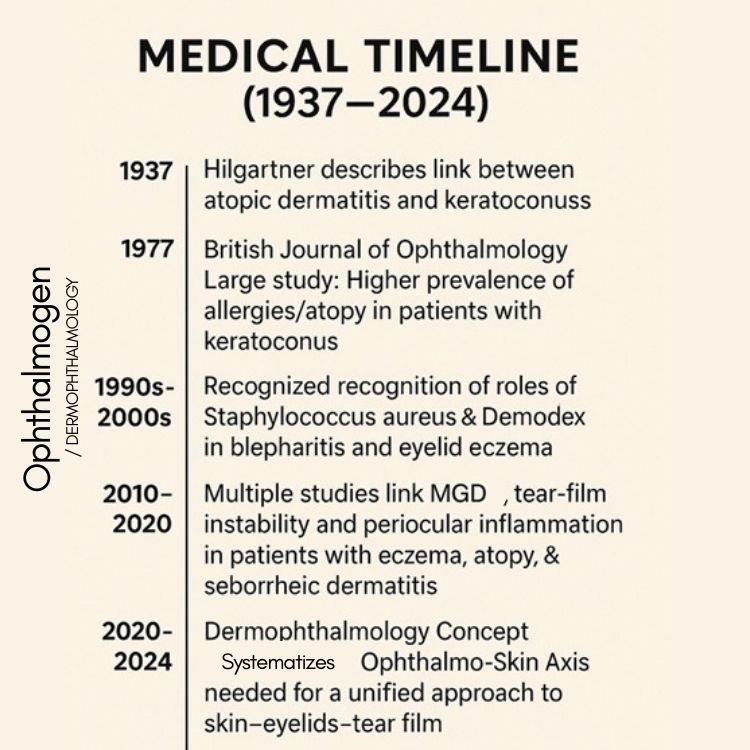
7. Dermophthalmology Medical Timeline
• 1937 – Hilgartner
First description of the link between atopic dermatitis and keratoconus.
• 1977 – British Journal of Ophthalmology
Large study showing higher prevalence of atopic/allergic tendencies in patients with keratoconus.
• 1990s–2000s
The roles of Staphylococcus aureus and Demodex in blepharitis and eczematous eyelid conditions become widely recognized.
• 2010–2020
Multiple studies connect MGD, tear-film instability, and periocular inflammation in patients with eczema, atopy, and seborrheic dermatitis.
• 2020–2025 – Dermophthalmology Concept
The idea of the Ophthalmo-Skin Axis is formalized and the need for an integrated skin–eyelid–tear-film approach (Dermophthalmology) is established
WOD – World Organization of Dermophthalmology: https://WOD.global
8. Treatment – The Dermophthalmology Approach
We treat simultaneously:
- Eyelid skin (eczema / dermatitis)
- Meibomian glands (MGD)
– Tear film
The most complete dermato-ocular solution today is the: Ophthalmogen Protocol
9. Full Ophthalmogen Protocol
(Ophthalmogen Eye10 – Ophthalmogen Gel – Ophthalmogen Spray)
STEP 1 — Ophthalmogen Eye10
Controlled heat at 40°C for 20 minutes
•opens Meibomian glands
•reduces inflammation
•stabilizes the tear film

STEP 2 — Ophthalmogen Gel
Massage Exfoliation – Demodex removal – Biofilm control
•removes scales
•helps reduce Demodex & bacterial load
•clears makeup residue from the lash line

STEP 3 — Ophthalmogen Spray
Hydration – Soothing – Antimicrobial action
• anti-Demodex
•balances the periocular skin microbiome
•supports tear film during the day

+ Visionlux Plus / Navitae Plus ophthalmic solutions & Flora Vision Spray artificial tears in spray form
For eczematous patients, advanced ocular surface hydration helps maintain a more stable tear film and visual comfort.
10. When will I see improvement?
•2–3 days → less irritation and burning
•1 week → reduced scaling on the lids
•2–3 weeks → more stable tear film, less fluctuating vision
•1 month → significantly fewer flare-ups

11. FAQ
Q1: Is eyelid eczema contagious?
No. Eczema is an inflammatory, not infectious, condition. However, microbes and Demodex can worsen the inflammation and symptoms.
Q2: Can eczema cause blurry vision?
Yes. Inflammation on the eyelids destabilizes the tear film, leading to fluctuating or blurry vision, especially on screens or in dry environments.
Q3: Is eczema linked with chalazia?
Yes. Chronic inflammation and MGD lead to blocked Meibomian glands, increasing the risk of chalazia.
Q4: Can makeup trigger flare-ups?
Yes, especially waterproof products and cosmetics containing fragrance or harsh preservatives. Proper lash-line cleansing and eyelid hygiene are essential.
Q5: What is the best daily routine for eyelid eczema?
Eye10 → Gel → Spray, 1–2 times per day, in coordination with your ophthalmologist and dermatologist.
Q6: Do I need to stop wearing contact lenses?
During intense flare-ups, many specialists recommend temporarily stopping contact lens wear until the ocular surface stabilizes.
Q7: When should I seek urgent medical care?
If you experience severe redness, pain, sudden visual loss, yellow crusts with pus, or signs of infection, you should be examined immediately.
12. Conclusion
Eyelid eczema:
• affects vision
• disrupts Meibomian gland function
• causes blepharitis & dry eye
• leads to recurrent flare-ups and discomfort
With Dermophthalmology as the guiding framework and the 3-Step Ophthalmogen Protocol, patients now have a complete, scientific, and safe solution for:
- healthy eyelids
- stable vision
- relief from inflammation
- daily prevention & long-term control