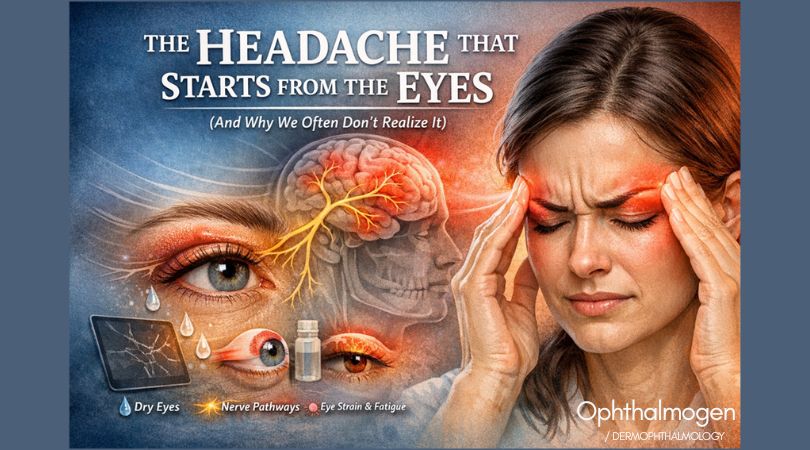
A headache that “starts from the eyes” is not an abstract idea.It has a specific mechanism — a clear beginning, middle, and end.And it almost always begins where most people never look:the eyelids and the eye’s microenvironment.
The eye is not only a vision organ — it’s a neurological system
Your eyes:
- are directly connected to the trigeminal nerve
- continuously send information to the brain
- require precise, constant, micro-coordinated function
This means something simple but crucial: When the eyes become fatigued, the brain “pays the price.”
Not necessarily with blur.But with:
- heaviness in the forehead
- pressure behind the eyes
- temple pain
- a “tight band” sensation
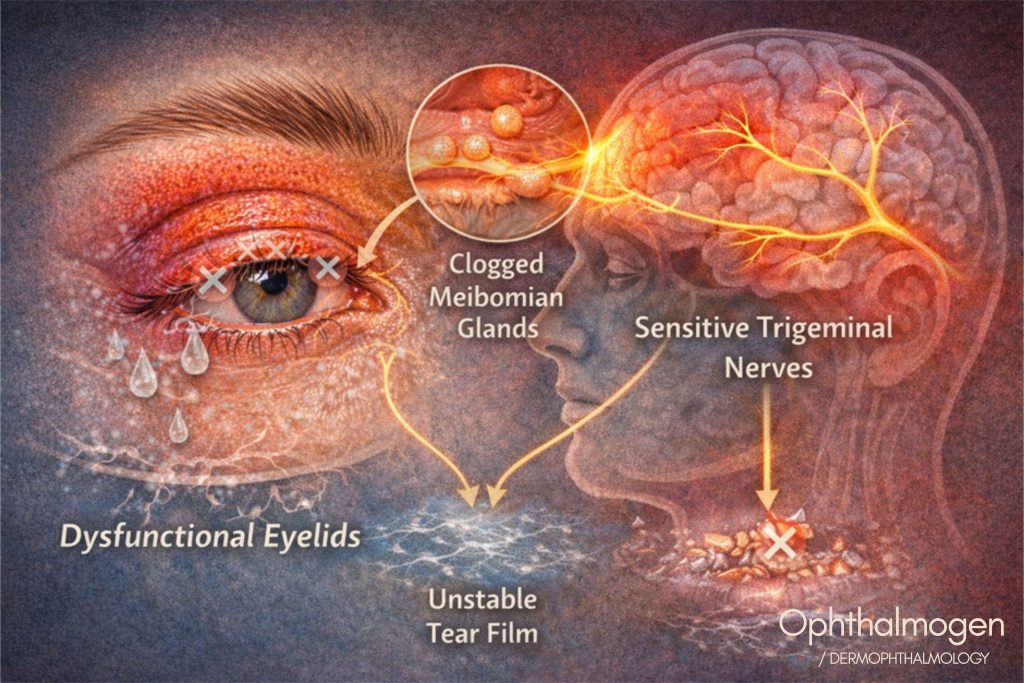
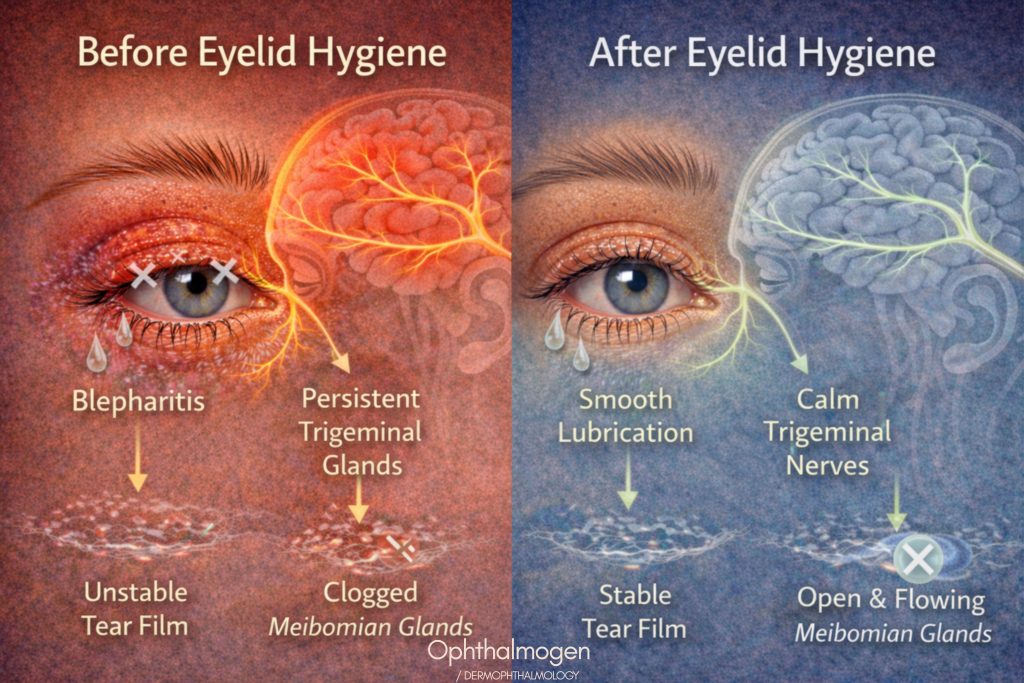
Everything begins with tear film instability
For the eye to feel comfortable, it needs:
- a stable tear film
- smooth lubrication
- proper distribution with each blink
But when:
- the eyelids are not cleaned properly
- the meibomian glands underperform
- the lipid layer is insufficient
then:
- tears evaporate too quickly
- the surface “micro-dries” in tiny, repeated episodes
- the eye works under stress
You don’t always experience this as “dry eye.”You experience it as fatigue.
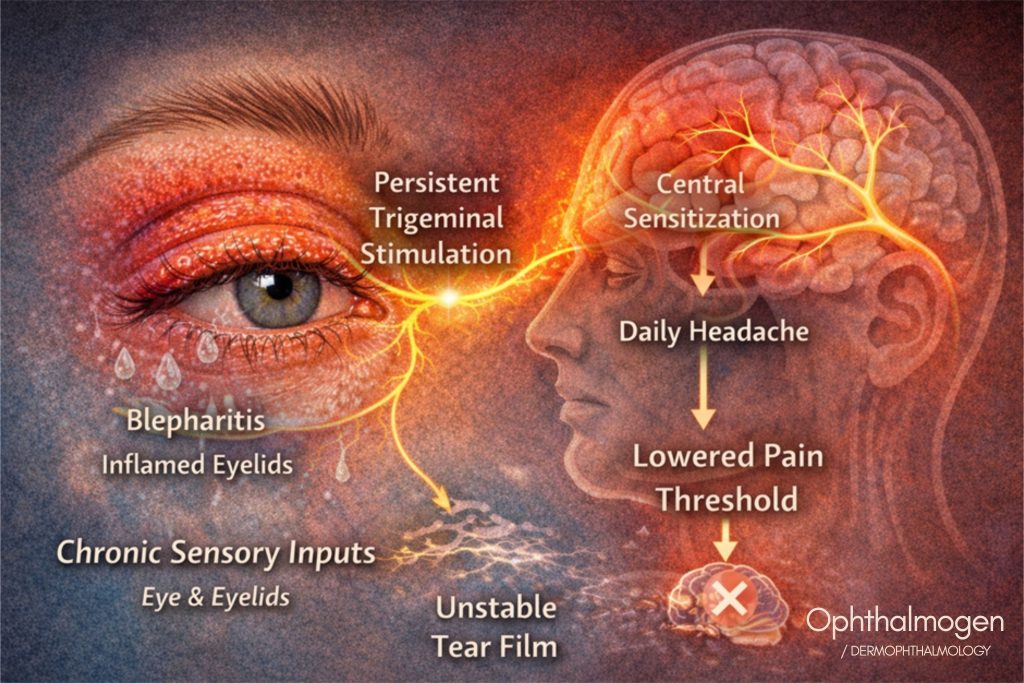
Low-grade eyelid inflammation becomes a constant stimulus.
Blepharitis, oiliness, secretions, Demodex, makeup residue.
All of these:
- create chronic low-grade inflammation
- irritate the area mechanically and chemically
- keep the system in a persistent “state of tension”
The trigeminal nerve doesn’t get a break.And when a nerve:
- is stimulated continuously
- without pauses
- without unloading
the brain translates that ongoing load into:tension-type headache (or a mixed pattern).
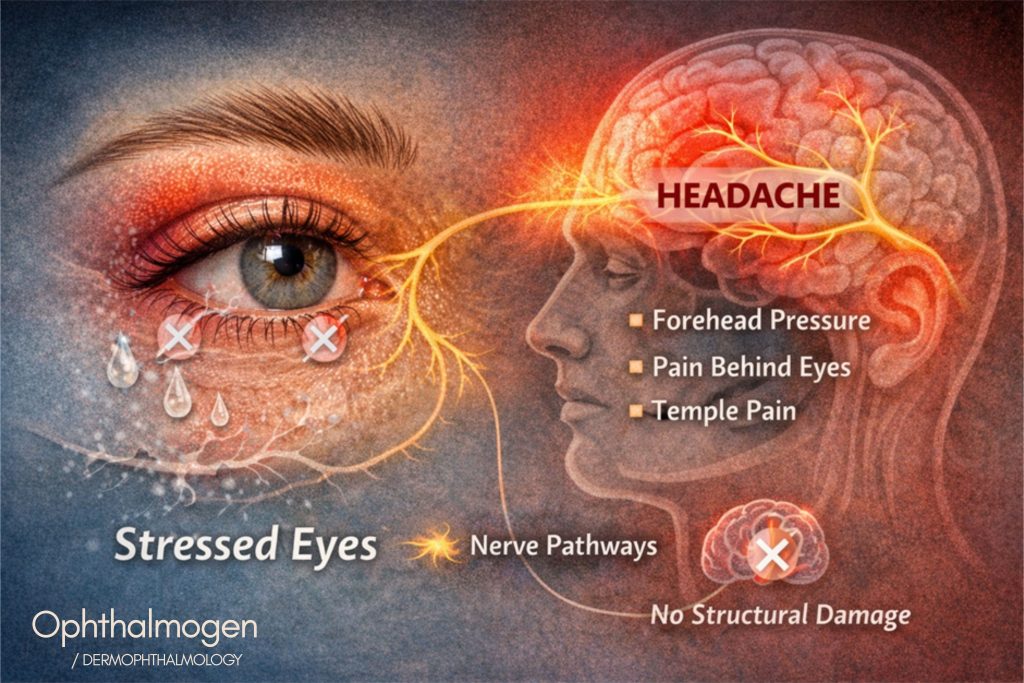
Integrated neurology insert: why this headache is real.
Modern Neurology recognizes that chronic, low-grade sensory input from the periphery (eyes, eyelids, face) can lead to:
- persistent trigeminal activation
- a lowered pain threshold
- central sensitization
- tension-type headache or mixed headache presentations
In other words:pain doesn’t require a visible “lesion” to exist.It requires continuous neural load.This explains why:
- the headache comes late in the day
- nothing “pathological” appears on tests
- simply closing the eyes can relieve it (reduced sensory load)
When the ocular system is unloaded (eyelids, tear film, blinking), the neural circuit stops being continuously provoked — and the headache has less reason to switch on.
The screen–blink vicious cycle.
When you look at a screen:
- blinking frequency decreases by up to 60%
- eyelids don’t “work” properly
- the tear film is not renewed
If your eyelids are already:
- tired
- inflamed
- functionally blocked
then every additional minute of screen time:
- increases neural load
- burdens the brain
- brings the headache closer
Why the headache appears late (not immediately)
This confuses most people.The headache:
- doesn’t arrive in the first hour
- comes at the end of the day
- or after several consecutive days of strain
Why?
Because:
- the system compensates
- until it crosses an adaptation threshold
Once that threshold is crossed, the brain “hits the brakes”in the only way it knows: pain.
That’s why your exams look “normal”
There is no:
- tumor
- lesion
- classic abnormal finding
There is:
- functional overload
- inflammation
- poor daily maintenance
Meaning: not a disease in the classic sense,but system dysfunction.
The key insight
A headache driven by the eyes:
- doesn’t start in the head
- starts at the eyelids
- travels through the tear film
- and ends in the nervous system
If you don’t unload the system at the source, you’ll keep chasing the symptom elsewhere.
When should you suspect your headache starts from the eyes?
You don’t need to be a doctor.Just answer honestly.
- If you say “yes” to 3–4 items, it’s not random.
- If you say “yes” to more, it’s very likely your headache isn’t only “in your head.”
Checklist: “That’s me”
The headache appears:
- toward the end of the day
- after many hours of screens
- not immediately upon waking
I feel:
- pressure behind the eyes
- tightness in the forehead or temples
- not “pounding,” but deepening fatigue
My eyes:
- tire easily
- feel heavier as the day goes on
- “can’t take it anymore” before the headache starts
I often have:
- mild stinging or burning
- dryness that’s not dramatic, but persistent
- a sense that “something is off,” without eye pain
The headache:
- improves when I close my eyes
- worsens with screens or bright light
- doesn’t permanently resolve with painkillers
I’ve noticed:
- I blink less when I work
- I “forget” my eyes during the day
- I do no daily eyelid care
I have a history of:
- blepharitis
- chalazion
- sensitive/irritated eyes
- dry eye (even mild)
My exams:
- are “clear”
- show nothing abnormal
- yet the headache persists
The most revealing sign
If your headache:
- isn’t always identical
- doesn’t come in distinct “attacks”
- feels like accumulated fatigue
then it’s not episodic neurological pain.It’s functional, daily overload.
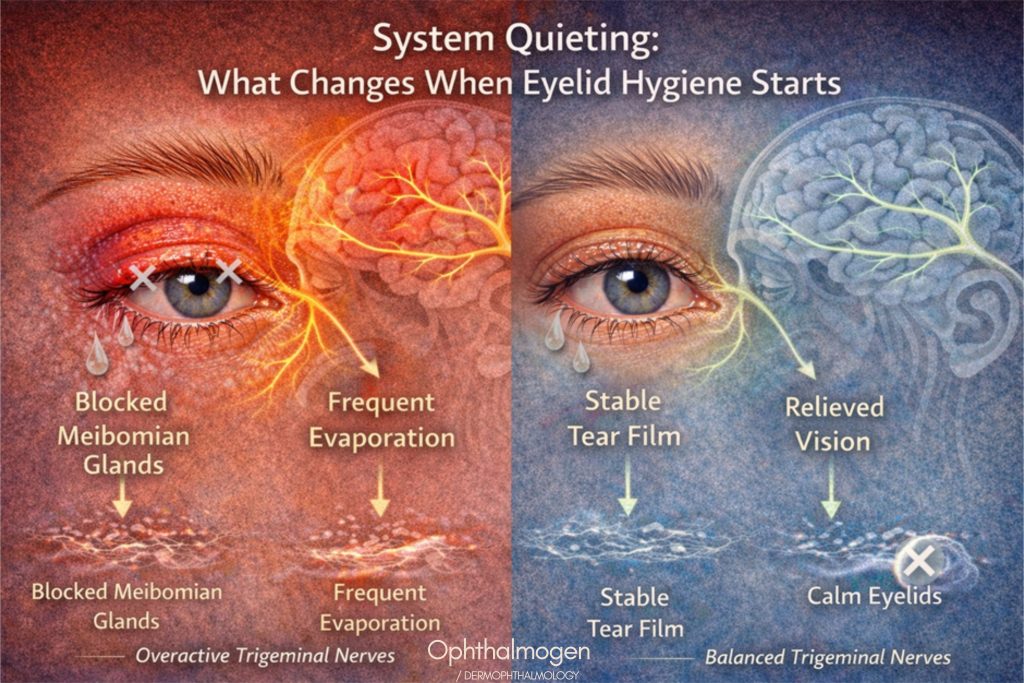
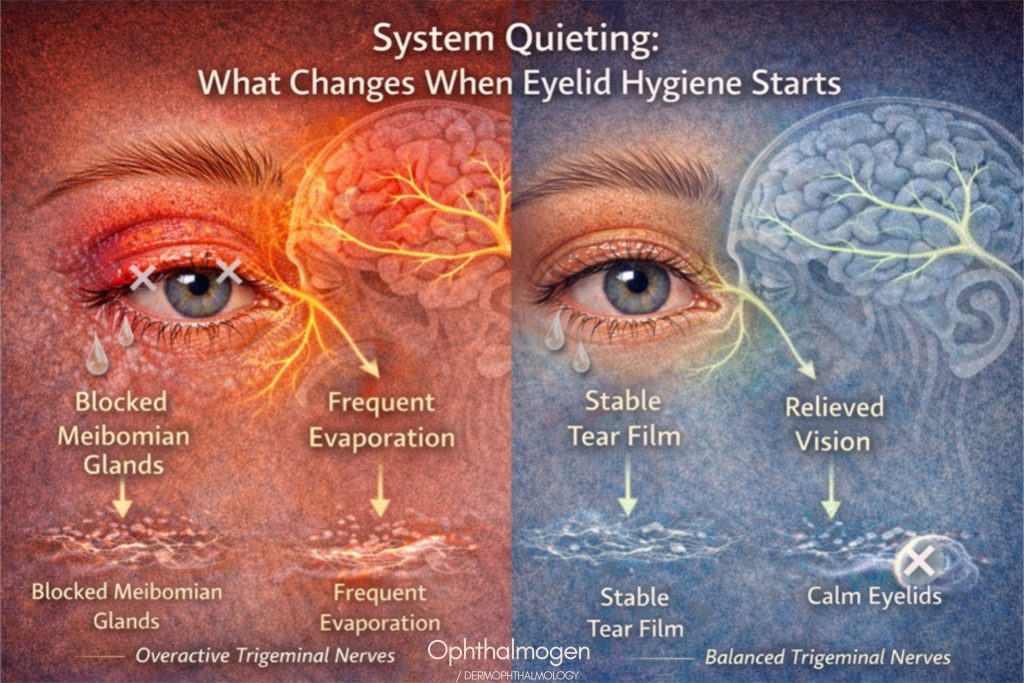
What changes when you care for the eyelids — not only the eyes.
(and why the headache fades without you chasing it)
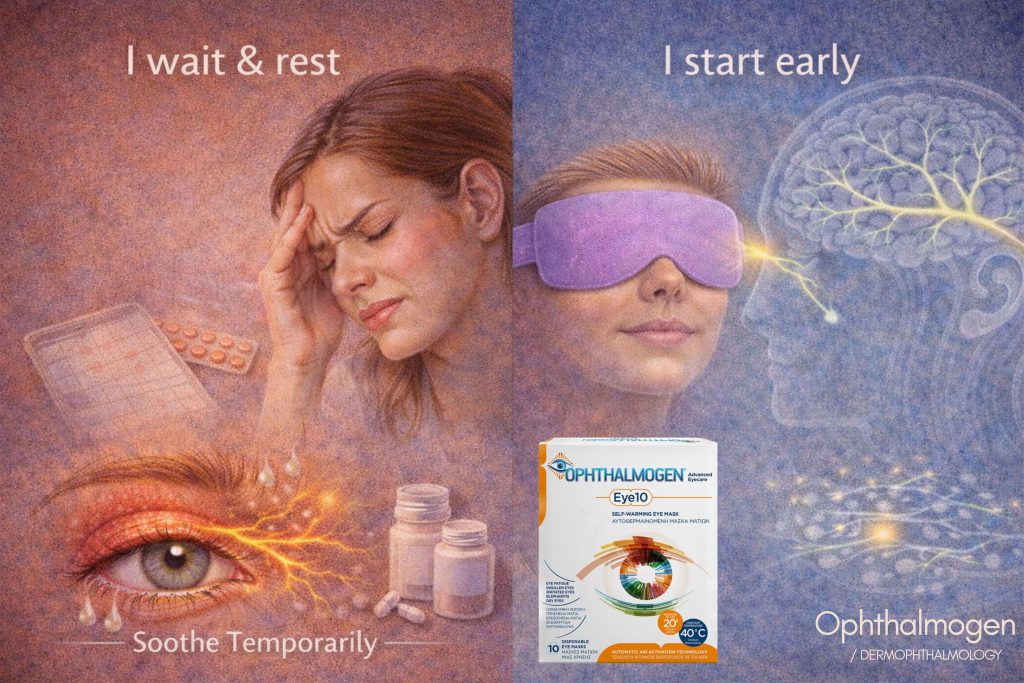
When people have headaches, they usually:
- close their eyes
- use drops
- take a painkiller
They feel better briefly.But the pattern returns.Why?Because the load often doesn’t start in the eyeball.It starts where most people ignore: the eyelids.
Eyelids are not “skin around the eye”
Eyelids are:
- the regulator of the tear film
- where the meibomian glands live
- the interface between vision, the nervous system, and daily strain
When eyelids are:
- inflamed
- stiff
- dysfunctional
- the eye works harder
- the brain receives continuous irritative input
- the headache builds gradually
What changes when you care for the eyelids — not only the eyes.
(and why the headache fades without you chasing it)
When people have headaches, they usually:
- close their eyes
- use drops
- take a painkiller
They feel better briefly.But the pattern returns.Why?Because the load often doesn’t start in the eyeball.It starts where most people ignore: the eyelids.
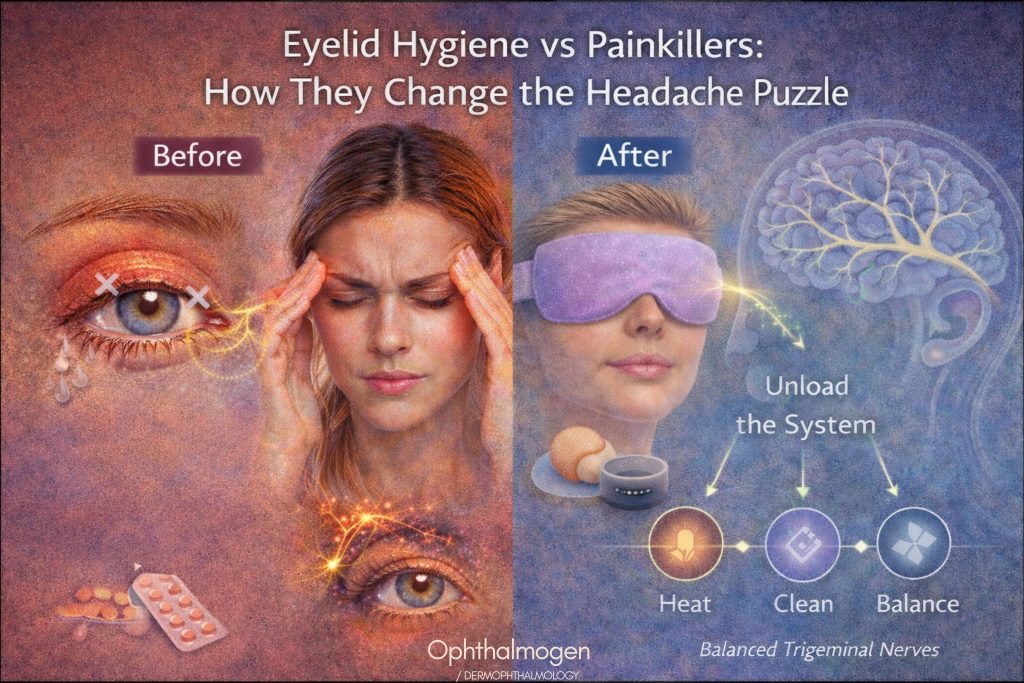
Controlled heat changes the game (cause-level, not symptom-level)
Controlled heat — such as what Ophthalmogen EYE10 provides — targets the cause, not only the sensation.What it actually does:
- liquefies thick meibomian secretions
- helps reopen glands that are functionally blocked
- restores lipid flow into the tear film
- relaxes periocular and forehead muscle tone
- less visual effort
- less neural stress
- fewer headaches
Not a “painkiller effect.”A progressive unloading effect.
You stop “chasing” the headache — it simply becomes less frequent
A classic sign you’re on the right track:
- it appears later
- it’s milder
- it comes less often
You’re not suppressing it.You’re weakening it at its source.
When, how, and how often to start eyelid hygiene
(and why the earlier you start, the less your headache “speaks”)
When to start
Short answer: before the headache arrives.Start when you notice:
- heaviness in the eyes
- forehead tension
- fatigue “climbing” toward the temples
or when:
- headaches recur
- appear during the day (not from morning)
- improve when you close your eyes
Don’t wait for a label.That’s when hygiene starts.
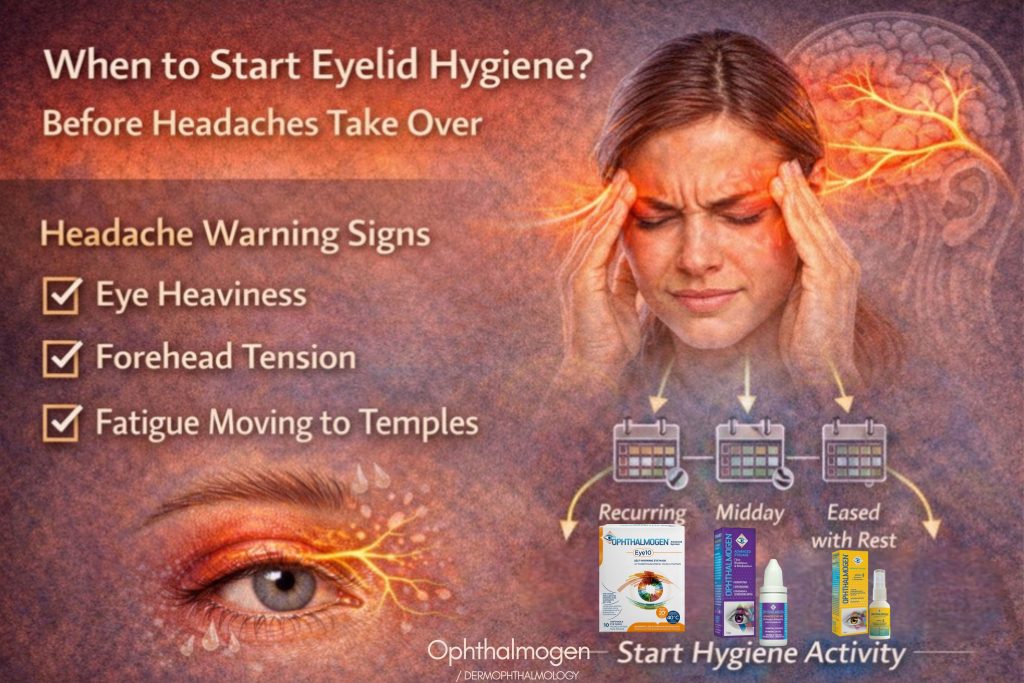
Why earlier is better
These headaches build quietly.Intervene early and you:
- reduce daily load
- prevent the brain from “learning” the stimulus
- reduce the chance of a chronic pattern
Like teeth: you don’t wait for gingivitis to brush.
How to do eyelid hygiene properly
Heat (the foundation)
Usually in the evening or after long screen time:
- prepares the eyelids
- softens secretions
- reduces muscular tone
Gentle activation & cleaning
After heat:
- no harsh rubbing
- no aggressive pressing
- no chasing “strong results”
Goal: restore function, not irritate tissue.
Daytime stability
For screens/AC/contact lenses:
- small interventions = less accumulation of irritation
How often ?
- Not “only when I hurt”.
- Not “whenever I remember”
Daily, like:
- washing your face
- brushing your teeth
This headache doesn’t want crisis treatment.It wants functional stability.
FAQ Frequently Asked Questions
- Should I stop my eye drops?
Not necessarily — and not abruptly.Drops can soothe, but they don’t unload eyelid dysfunction. With consistent eyelid care, many people:
- need fewer drops
- use them less often
- feel longer-lasting relief
- Is this for everyone?
It helps especially when headache is linked to screens, fatigue, dryness, or “pressure behind the eyes.”It is not a solution for sudden severe headaches of unknown cause, or headaches with neurological red flags. In those cases, medical evaluation comes first.
- When will I notice a difference?
Usually:
- first days: less eye tension
- 1–2 weeks: fewer headaches
- 3–4 weeks: greater stability and less need for “support”
- If I’m not in pain now, does it still matter?
Yes — that’s when it matters most.This is load prevention, not crisis management.
Scientific insert (updated): why this aligns with modern evidence
The idea that headaches can originate from the eyes/eyelids is increasingly supported.
Visual fatigue & headache
Screens + reduced blinking + tear film instability correlate with frontal/temporal headache and pressure sensations.
Dry eye as homeostasis disruption
TFOS DEWS II defines dry eye as a tear film homeostasis disorder, not simply “not enough tears.”
Blepharitis & MGD
MGD and chronic lid inflammation lead to poor tear film quality → irritation → functional load.
Trigeminal pathways (shared neural network)
Eyes, eyelids, forehead, and temples share trigeminal pathways → ocular irritation can be perceived as headache.
Central sensitization
Neuroscience shows chronic sensory input can lower pain thresholds and maintain headache without visible damage —
matching the “accumulated fatigue headache” described here.
Mini References List
- Jones L, Downie LE, Korb D, et al. (2017). TFOS DEWS II Management and Therapy Report. The Ocular Surface.
- Craig JP, Nichols KK, Akpek EK, et al. (2017). TFOS DEWS II Definition and Classification Report. The Ocular Surface.
- Rosenfield M. (2016). Computer vision syndrome: a review. Ophthalmic and Physiological Optics.
- Foulks GN, Nichols KK. (2016). Meibomian gland dysfunction and evaporative dry eye. Ophthalmology.
Neurology add-on:
- Woolf CJ. (2011). Central sensitization: implications for diagnosis and treatment of pain. Pain.
- Goadsby PJ, Holland PR, Martins-Oliveira M, et al. (2017). Pathophysiology of migraine: a disorder of sensory processing. Physiological Reviews.
Scientific Disclaimer
This article is for informational purposes and does not replace medical diagnosis or individualized treatment. If your headache is sudden, severe, different from usual, or accompanied by neurological symptoms (e.g., weakness, numbness, speech/vision changes), seek urgent medical evaluation.
Call–to–action
If you recognized yourself in the checklist, don’t focus only on “what to take for the headache.”The most useful step is to identify where the load starts.Consistent eyelid care — especially strategies that stabilize the tear film and use controlled heat — can change the daily fatigue pattern and, with it, reduce headache frequency.