Headache is one of the most common symptoms of modern life.And for most people, the explanation comes almost automatically:“Fatigue,” “Stress,” “Migraine.”
Yet in recent years, scientific evidence has been pointing to something different — and for many people, something relieving:that in individuals with dry eye disease and blepharitis,headache is often not an independent symptom,but part of the same functional disorder.
And this is exactly where the Eye–Skin Axis comes into play.
A Eye–SkinAxis: Why Eyes and Eyelids Do Not Function Independently.
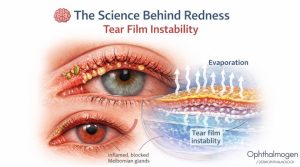
The modern term Eye–Skin Axis describes something clinical practice has observed for years, but had not clearly named:that the eyelid skin, eyelashes, glands, and ocular surface form a single, integrated functional system. When the cutaneous microenvironment of the eyelids is disrupted:
- inflammation
- excess oiliness
- Demodex
- makeup residue
- meibomian gland dysfunction (MGD)
the ocular surface is also disrupted and, ultimately, the nervous system becomes burdened.
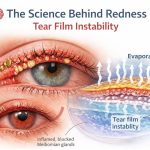
Dry Eye & Headache: A Shared Pathophysiological Substrate.
According to the major TFOS DEWS II reviews (The Ocular Surface, 2017):
- dry eye disease is not simply a lack of tears
- it is a disorder of tear film homeostasis and stability
breaks up rapidly
- breaks up quickly
- lacks adequate lipid support
- is not renewed with each blink
then:
- the ocular surface becomes intermittently irritated
- the eye sends continuous discomfort signals
- the brain perceives these signals as fatigue
And this fatigue is often expressed clinically as tension-type headache.
This is why many people with dry eye:
- experience headaches
- despite normal imaging and examinations
- and without a formal “neurological diagnosis”
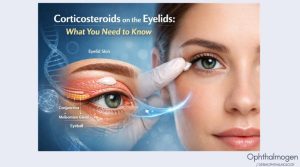
Blepharitis & MGD: The Overlooked Link.
Chronic eyelid inflammation and meibomian gland dysfunction:
- degrade the lipid layer of the tear film
- increase tear evaporation
- force the eye to function under constant strain
Wherever continuous muscular and neural tension exists, headache finds fertile ground.Here, blepharitis is not merely a local condition.It is a central component of the Eye–SkinAxis.
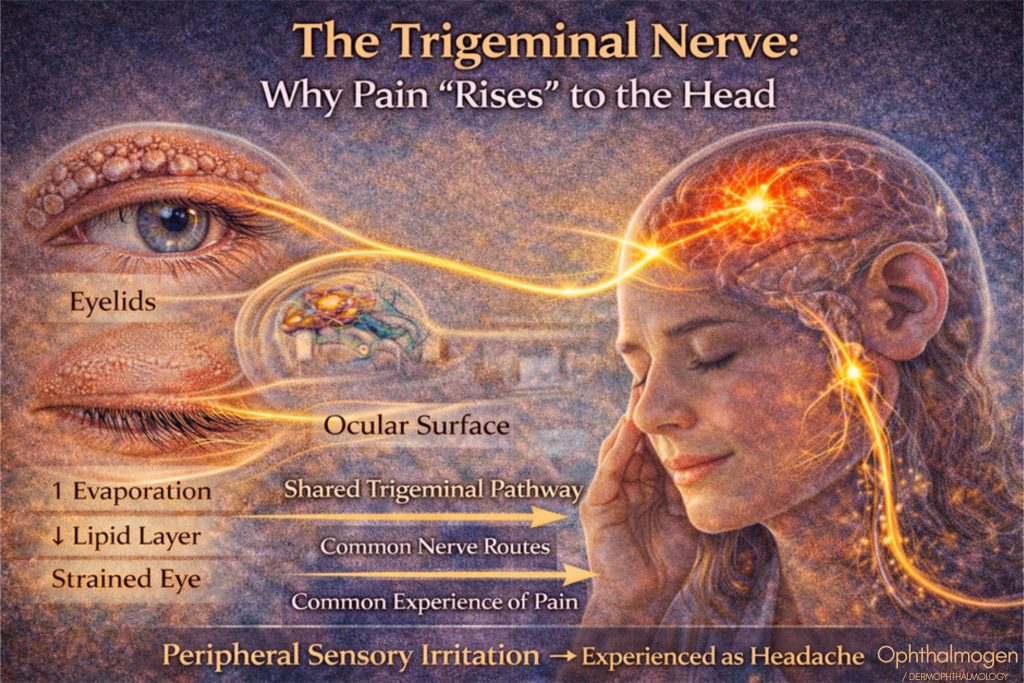
The Trigeminal Nerve: Why Pain “Rises” to the Head.
Anatomically:
- eyes
- eyelids
- forehead
- temples
share common neural pathways through the trigeminal nerve.
This leads to a crucial insight: Irritation at the eyelids or ocular surface → may be perceived as headache. Not because the problem “is in the head,” but because the neural network is shared.
Modern neurology (Goadsby et al., Physiological Reviews) recognizes that:
- peripheral sensory stimuli
- can maintain or trigger headache
- without structural damage
Scientific Validation
Why This Is Not a Hypothesis, but a Convergence of Disciplines
In recent years, ophthalmology, neurology, and pain science have converged on a shared understanding:chronic, low-grade peripheral sensory stimulationcan maintain or provoke headachewithout structural pathology.
In dry eye disease and blepharitis, this stimulation:
- originates in the Eye–Skin Axis
- is transmitted via the trigeminal nerve
- and manifests as tension-type or mixed headache
This explains why:
- imaging studies are normal
- analgesics offer temporary relief
(paracetamol, ibuprofen, aspirin, NSAIDs)
- but symptoms recur as long as the stimulus persists.
Painkillers suppress the symptom, they do not remove the source of neural load.
Why Tests Are “Normal” but the Headache Persists.
In these cases, there is:
- no tumor
- no lesion
- no pathological imaging finding
There is:
- functional overload
- microinflammation
- chronic sensory stimulation
In other words: not disease, but system dysfunction. This fully aligns with the concept of central sensitization (Woolf CJ, Pain, 2011). centralsensitization (WoolfCJ, Pain, 2011).
What Changes When You Care for the Eyelids.
(Eye–SkinAxis in Practice)
When care is limited to eye drops alone:
- the ocular surface may feel better
- but the system remains overloaded
When the entire Eye–Skin Axis is addressed:
- eyelids
- eyelashes
- glands
- the tear film
neural load decreases and headache frequency diminishes.
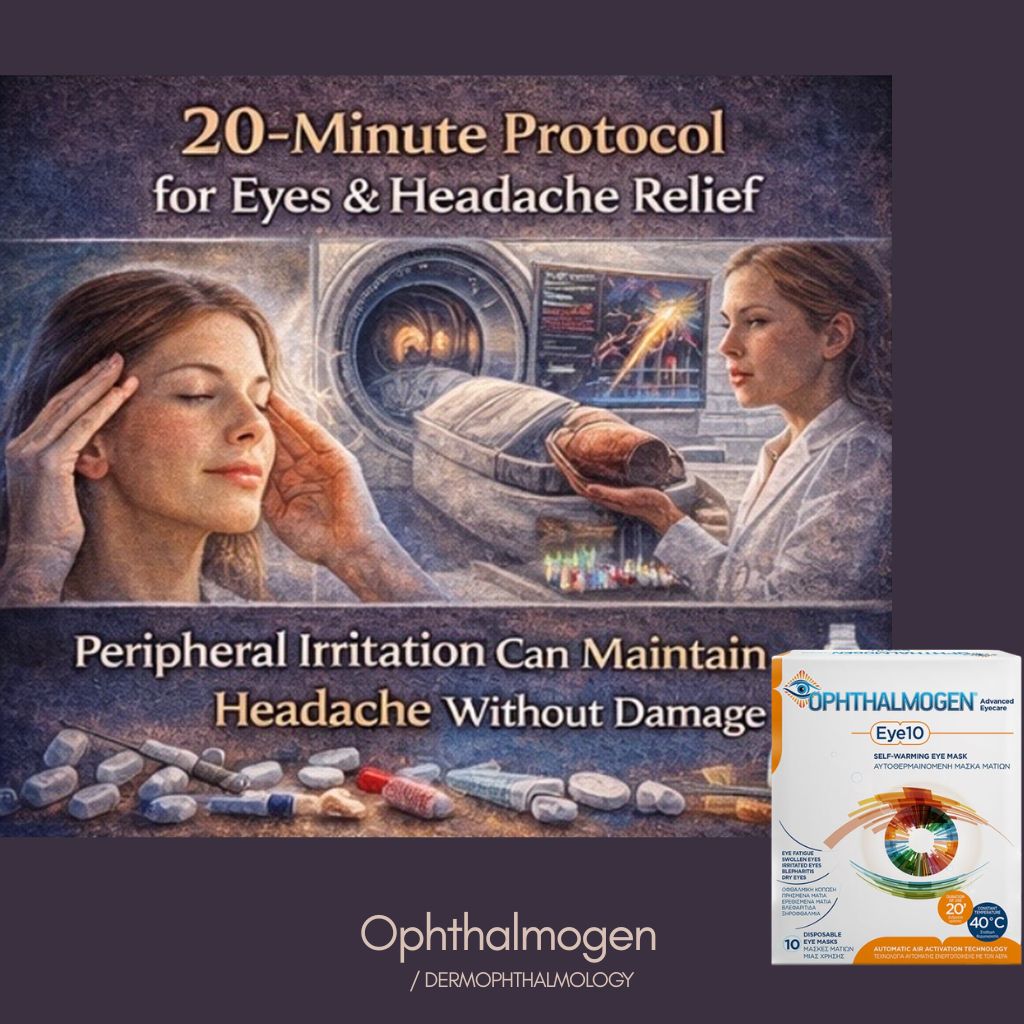
A 20-Minute Practical Protocol for Eyes & Headache
Controlled heat – Ophthalmogen EYE10
- 20 minutes
- liquefies gland secretions
- relieves meibomian gland obstruction
- relaxes periocular and forehead muscle tone
- alleviates visual fatigue
Gentle eyelid massage – Ophthalmogen Gel
- Activates natural gland expression
- reduces stagnation
- improves blinking mechanics
- relieves ocular strain
This is not relaxation — it is functional decompression.
Daily eyelid spray – Ophthalmogen Spray
- hydrates eyelid skin and lashes
- reduces Eye–Skin Axis microinflammation
- supports daily stability (screens, air conditioning)
Vitamin B12 artificial tears – Visionlux Plus Duo
- stabilize the tear film
- enhance ocular surface resilience
- reduce the “neural fatigue signal”
- vitamin B12 supports cellular metabolic function
You are not chasing the headache. You are removing the stimulus that creates it.

In Summary
If you have dry eye or blepharitis and you also experience headaches, it is not necessarily a coincidence. it is often the same functional problem. And when you care for the Eye–Skin Axis:
- the system unloads
- and the headache loses its foundation.
Scientific Disclaimer
This article is for informational purposes only and does not replace medical diagnosis or individualized treatment.
Sudden, severe, or unusual headaches require immediate medical evaluation.