Introduction
Diabetes mellitus is a chronic metabolic disease that affects multiple systems of the body. One of the frequent but often overlooked problems in diabetic patients is the increased predisposition to eyelid conditions, most notably chalazion.
Chalazion, a chronic inflammatory cyst of the eyelid, is not just an aesthetic concern – it can affect vision quality and daily life. In diabetic patients it occurs more often, tends to recur, and heals more slowly.
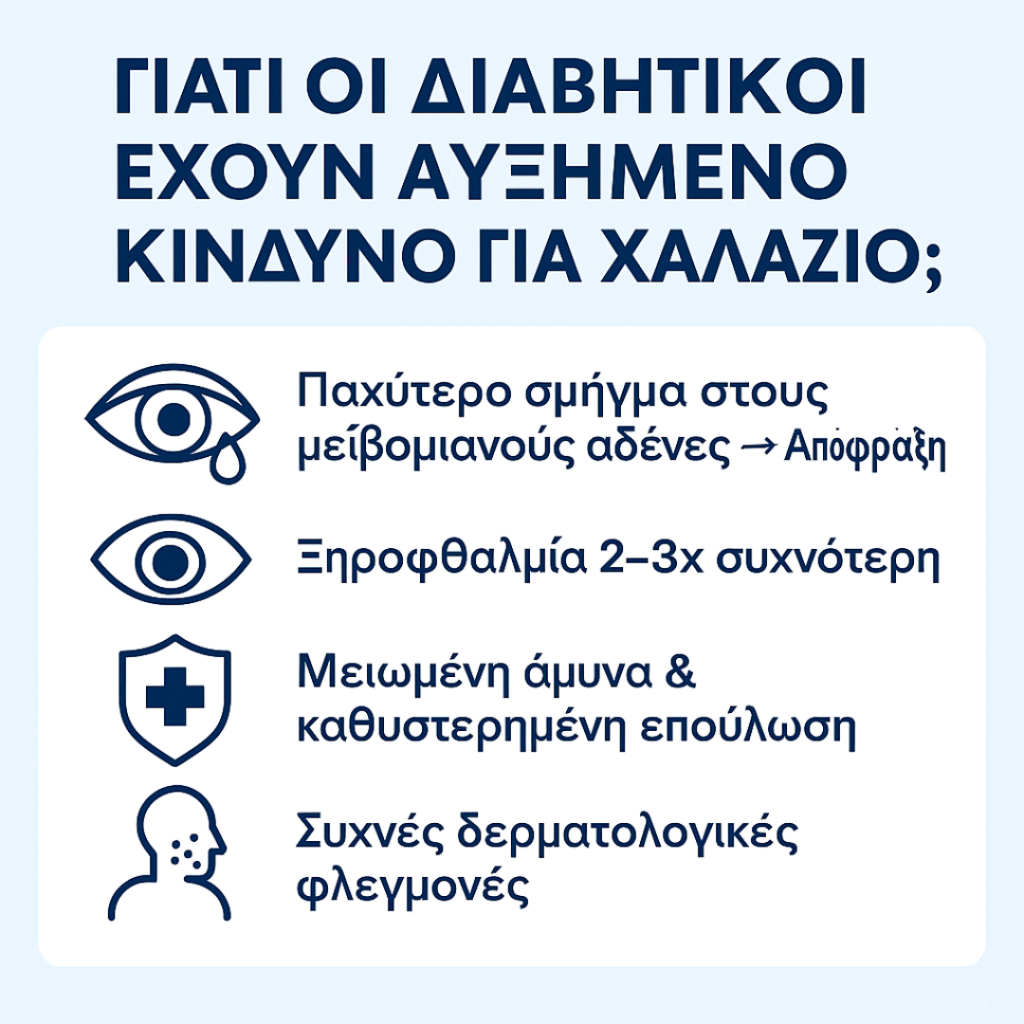
Why Do Diabetic Patients Have Increased Risk of Chalazion?
- Impaired Meibomian Gland Function
Diabetes affects the quality of the lipids secreted by the Meibomian Glands. The result is thicker meibum, which clogs the gland openings and leads to chalazion formation.
- Dry Eye and Tear Film Instability
Dry eye is 2–3 times more common in diabetics due to neuropathy and angiopathy. The destabilized tear film promotes inflammation and gland obstruction.
- Reduced Immunity and Delayed Healing
In diabetic patients, minor inflammations and infections last longer. This means a simple chalazion may persist for weeks, recur, or be complicated by conjunctivitis.
- Associated Skin Conditions
Diabetics are more prone to dermatitis and skin infections, which can also affect the eyelids.
Statistics
- Diabetics have twice the risk of developing chalazion compared to the general population.
- 30–40% of diabetics with chronic blepharitis will develop recurrent chalazia.
- Women with diabetes who use makeup have up to 3 times higher risk.
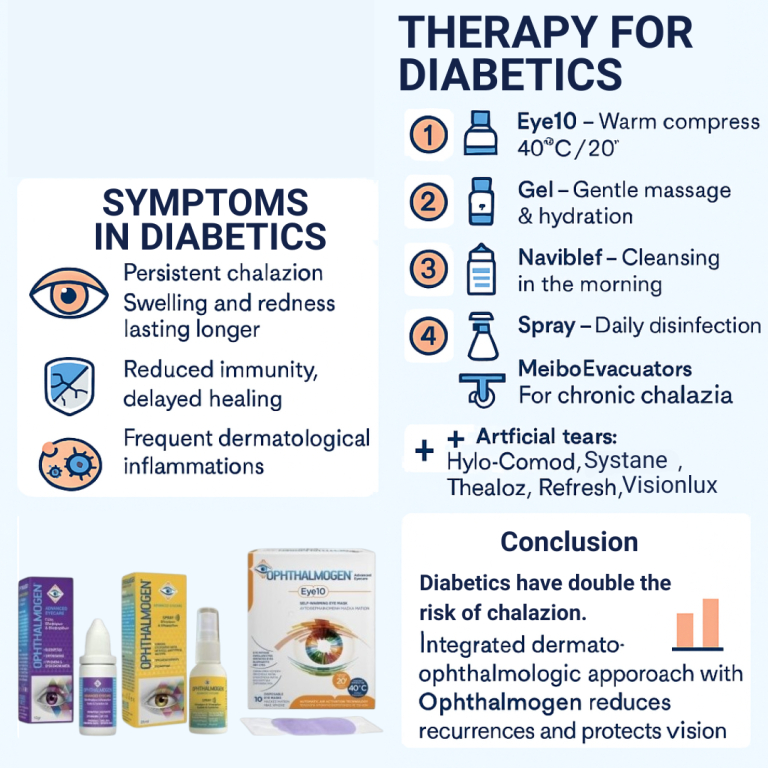
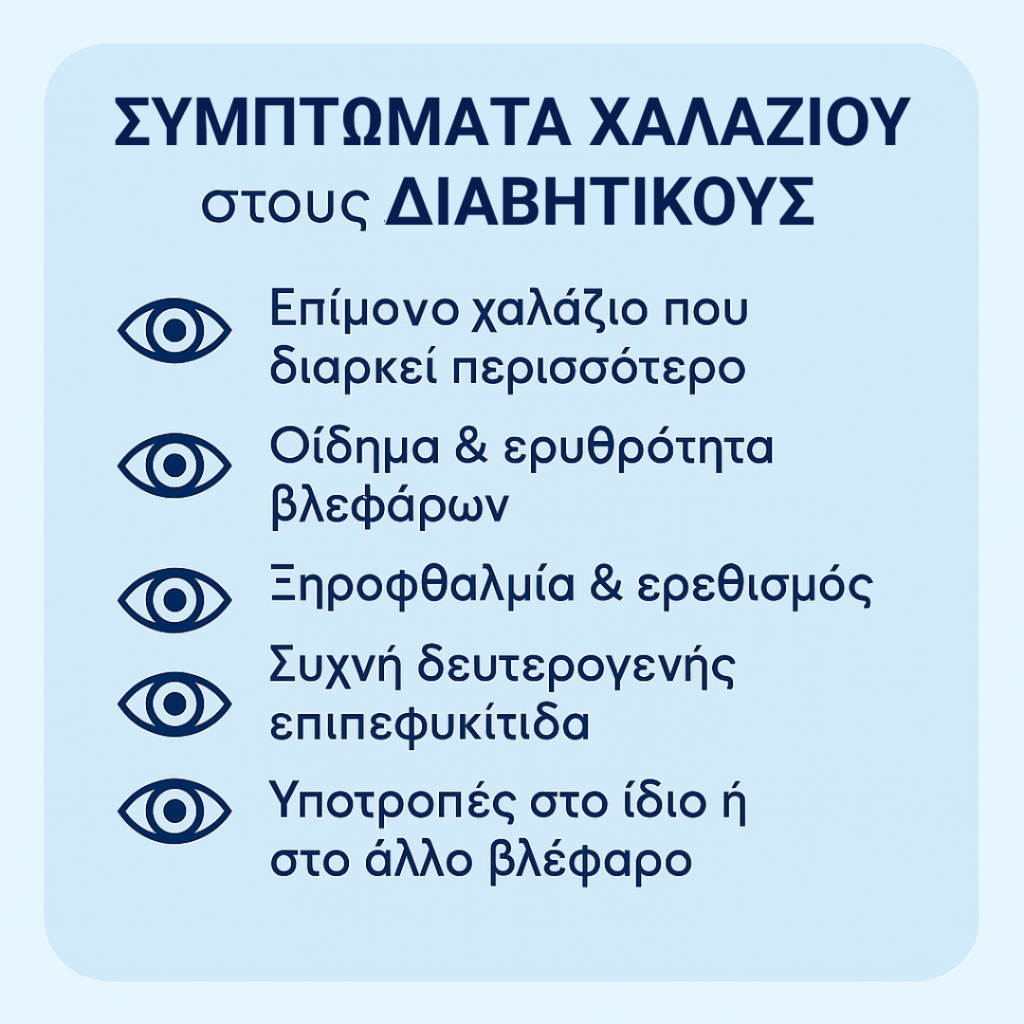
Symptoms in Diabetic Patients
The classic symptoms of chalazion (eyelid swelling, redness, firm lump) are often more pronounced in diabetics and typically:
- Last longer.
- Are accompanied by dry eye or irritation.
- Sometimes lead to secondary conjunctivitis.
Chalazion and Complications in Diabetic Patients
- Recurrence: Chalazion can repeatedly appear in the same or opposite eyelid.
- Secondary infections: Due to impaired immunity.
- Eyelash changes: Madarosis (loss), trichiasis (misdirection), dystrophy.
- Reduced vision: If chalazion presses on the cornea.
Prevention – Comprehensive Dermophthalmology Care
The best strategy for diabetics is daily eyelid and eye care, based on the dermophthalmology approach.
Step 1: Thermotherapy with OphthalmogenEye10
- 20 minutes at 40°C melts the thickened meibum.
- Especially helpful in patients with MGD and diabetes.
Step 2: Massage with OphthalmogenGel
- Applied after thermotherapy, allows gentle massage without friction.
- Helps unclog glands and reduces inflammation.
Step 3: Cleansing with Naviblef
- Απομάκρυνση μικροβίων, λιπαρότητας και Demodex.
- Ιδανικό για χρήση κάθε πρωί.
Step 4: Hydration with Ophthalmogen Spray
- Applied during the day for disinfection and hydration.
- It contributes to the control of dry eyes.
- Supports dry eye control.
Step 5: Artificial Tears
- Navitae Plus, Hylo-Comod, Systane, Thealoz, Refresh, Visionlux Plus.
- Stabilize the tear film.
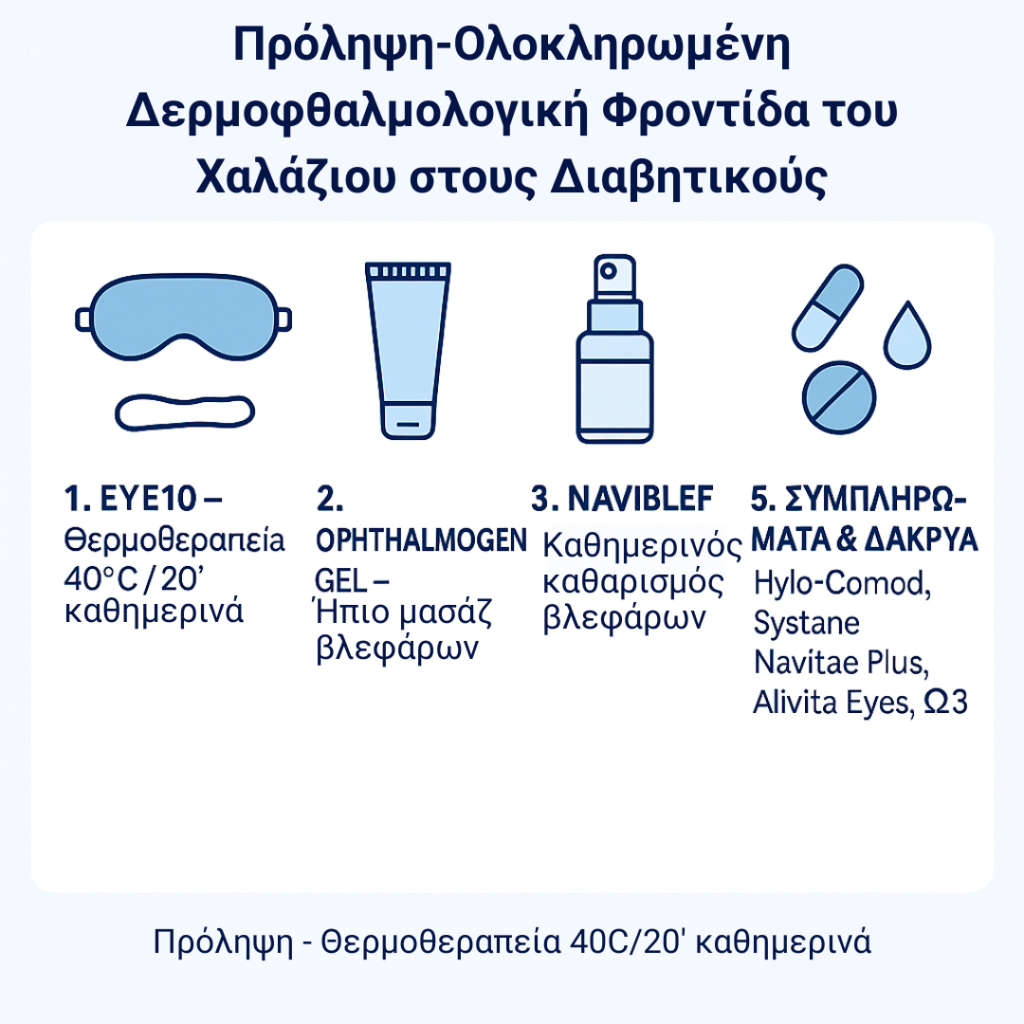
Step 6: Nutritional Supplements
- Ω-3: Allvita Eyes,Solgar, Minami, Lamberts.
- Reduce inflammation, improve tear film lipid quality.
Medical Support (if needed)
The ophthalmologist may prescribe topical therapy in difficult cases:
- Tobradex or Dexamytrex for inflammation/infection.
- Antibiotic or corticosteroid drops for conjunctivitis.
In Summary
Chalazion is common in diabetic patients, linked to changes in skin, tear film, and reduced immune defense.
Comprehensive care with Ophthalmogen (Eye10, Gel, Naviblef, Spray, MeiboEvacuators), combined with artificial tears and omega-3 supplements, offers the most effective prevention and management, reducing recurrences and improving quality of life.
- Dermophthalmology provides diabetic patients with a new perspective: care not only for the eyes, but for the entire skin–eyelid–ocular microenvironment

Dermophthalmology is the new medical specialty we have introduced (learn more at www.dermophthalmology.com)