Introduction
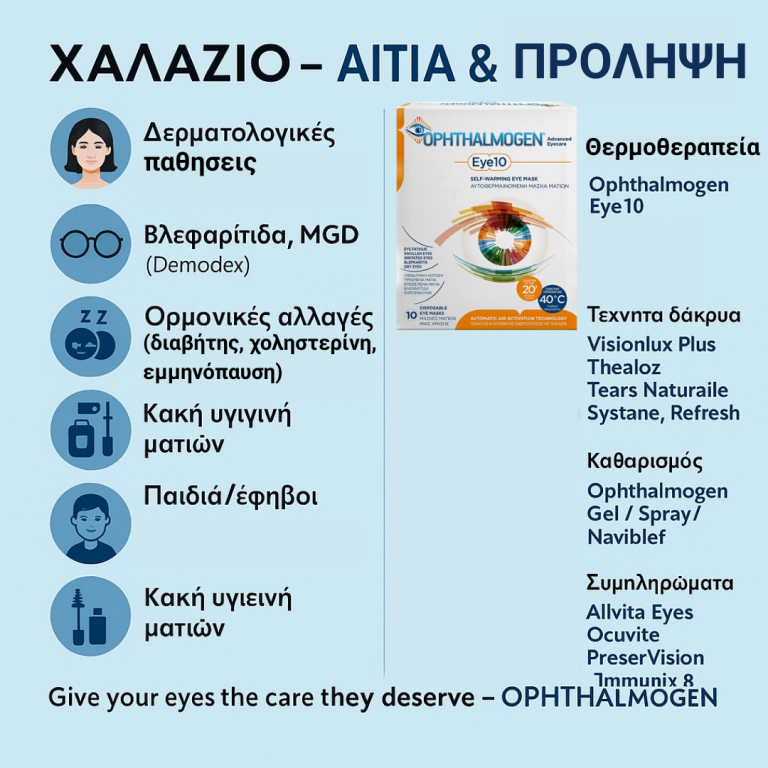
Chalazion is one of the most common eyelid problems. It is a chronic inflammatory cyst that develops on the eyelid due to obstruction of the Meibomian Glands – the small glands that produce the oily component of the tear film. While not dangerous to vision, chalazia are often bothersome, tend to recur, and can affect both appearance and ocular comfort.
Modern medicine no longer limits chalazion management to drug therapy or minor surgery. Instead, it considers the entire dermo-ophthalmic microenvironment: the skin, eyelids, eyelashes, and ocular surface. This holistic perspective has given rise to Dermophthalmology – a new interdisciplinary field combining Dermatology and Ophthalmology, revolutionizing the prevention and treatment of conditions such as chalazion.
Statistics Statistics:
- 8–10% of the population develop a chalazion each year.
- 20% of adults will experience at least one chalazion in their lifetime.
- 2–5% of children are affected, often due to poor hygiene or eye rubbing.
- 25–30% of patients with rosacea or seborrheic dermatitis develop chalazia.
- Women using daily eye makeup → 40% higher risk.
- Patients with glaucoma or cataract (long-term drops, ocular surface problems) → significantly increased risk.
Why Do Diabetic Patients Have Increased Risk of Chalazion?
- Meibomian Gland Dysfunction (MGD)
The leading cause. Thickened meibum blocks the gland openings, forming a cyst.
- regulation
Microscopic mites (Demodex folliculorum/brevis) colonize eyelashes and are linked to chronic blepharitis, a major chalazion risk factor.
- Dermatological Conditions
- Rosacea
- Seborrheic dermatitis
- Psoriasis
- Keratotic skin disorders
Residual mascara and eyeliner clog gland orifices. Eyelash extensions increase risk of bacterial growth and Demodex infestation.
- Hormonal and Environmental Factors
- Adolescence: higher sebaceous activity.
- Pregnancy & menopause: hormonal changes affect tear composition.
- Men over 50: reduced androgens worsen MGD.
- Lifestyle: poor sleep, diet, stress, and pollution aggravate risk.
Less frequent but often recurrent due to:
- Frequent eye rubbing.
- Allergies leading to eyelid irritation.
- Inadequate eyelid hygiene.
- Prolonged use of contact lenses alters the tear film.
- Alter tear film, reduce blinking → stagnant meibum → gland obstruction.
- Solutions with preservatives may irritate eyelids.
- Diabetic Patients
- Twice the risk due to poor wound healing and dry eye.
- Higher predisposition to infections.
- Patients (High Cholesterol/Triglycerides)
- Leads to thicker meibum.
- Increases risk of obstruction.
- Immunosuppressed Patients
- Post-transplant, chemotherapy, or chronic steroid therapy → higher risk.
- Increased risk due to reduced defense.
- Prolonged use of computers and mobile phones reduces blinking.
Reduced blinking during screen time → tear film stagnation → blocked glands.

Symptoms and Diagnosis
- Eyelid swelling.
- Hard lump (pea-like nodule).
- Mild or no pain.
- Blurred vision if pressing on the cornea.
Diagnosis is clinical by an ophthalmologist.
Why Does Chalazion Recur?
The classic symptoms of chalazion (eyelid swelling, redness, firm lump) are often more pronounced in diabetics and typically:
- Persistent Meibomian gland dysfunction.
- Chronic blepharitis.
- Lack of consistent eyelid hygiene.
- Skin type predisposition (rosacea, seborrhea, acne).
The New Dermophthalmology Approach
Dermophthalmologycombines Ophthalmology + Dermatology, recognizing that the eye and skin share embryological origin (ectoderm).
Key points:
- Skin type affects ocular comfort.
- Dermatological conditions increase chalazion risk.
- Daily eyelid hygiene and Demodex control are essential.
Treatment and Daily Care
The modern therapeutic sequence is::
- Ophthalmogen Eye10 – Thermal therapy at 40°C for 20 minutes once daily for 1 month.
- Massage with Ophthalmogen Gel – Gentle gland expression and eyelid hydration.
- Morning cleansing with Naviblef foam and lukewarm water.
- Ophthalmogen Spray during the day – eyelid disinfection and Demodex control.
- OphthalmogenMeiboEvacuators – for chronic blepharitis with recurrent chalazia.

Adjunctive Medical Therapy
In resistant or inflamed cases, ophthalmologists may prescribe steroid/antibiotic drops or ointments such as:
- Tobradex
- Dexamytrex
Their use should only be done under medical guidance.
Essential for hydration and tear film stability.
Brands: Navitae Plus, Hylo-Comod, Thealoz Duo, Systane, Refresh, Artelac, Tears Naturalle, Visionlux Plus.
Nutritional Supplements (Omega-3 and Antioxidants)
Daily Omega-3 intake improves meibum quality and reduces inflammation.
SEO-relevant brands:
- Minami MorEPA
- Solgar Omega-3
- Lamberts Omega-3
- Opti3 Omega-3 (φυτικής προέλευσης)
- Allvita Eyes (πλήρεςσκεύασμαγια AMD &ξηροφθαλμία)
MacuShield&MacuSave (μελουτεΐνη, ζεαξανθίνη, μεσοζεαξανθίνη).
Chalazion and Eyelashes
Chalazion, through chronic blepharitis and MGD, affects eyelash health:
- Madarosis (loss of lashes): localized around recurrent chalazia.
- Trichiasis: lashes turn inward due to scarring, irritating the cornea.
- Eyelash dystrophy: fragile, irregular lash growth.
- Alopecia: rare, associated with alopecia areata.
Proper care with Ophthalmogen Spray, Naviblef, Eye10, and Gel massage reduces recurrences and maintains healthy eyelashes.

Chalazion and Conjunctivitis
Chalazion itself is not contagious and not an infection. But it can be associated with conjunctivitis:
- Secondary bacterial conjunctivitis if chalazion becomes infected (usually staphylococcal).
- Chronic blepharitis and MGD → common causes of recurrent conjunctivitis.
- In children, poor hygiene and eye rubbing lead to chalazion plus conjunctivitis.
Management:
- Eyelid hygiene (Naviblef, Ophthalmogen Spray).
- Eye10 thermal therapy + Gel massage.
- If conjunctivitis is present → prescribed drops (Tobradex, Dexamytrex).

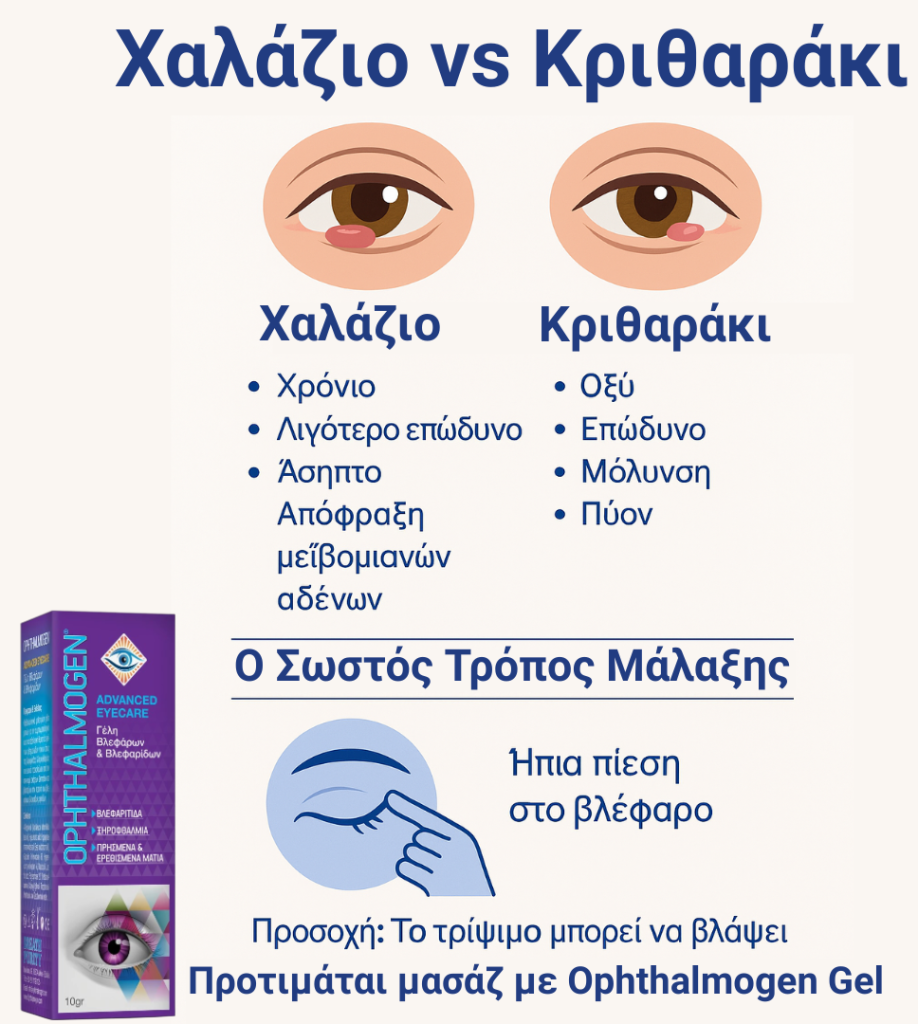
Chalazion vs Stye (Hordeolum)
Many confuse chalazion with stye:
- Stye: acute, painful, pus-filled, due to infection
- Chalazion: chronic, less painful, sterile
A stye can evolve into a chalazion, but a chalazion is not infectious.
Eyelid massage
After thermal therapy, gentle eyelid massage is vital to express meibomian secretions.
- Avoid vigorous rubbing (may damage eyelids).
- Ophthalmogen Gel massage is safe and effective
Frequently Asked Questions (FAQ)
How long does chalazion last?
2–6 weeks typically.
Is it contagious?
No.
When is surgery required?
For persistent, large chalazia unresponsive to therapy.
Does it recur?
Yes, especially in blepharitis, diabetes, dyslipidemia, or contact lens wearers.
In Summary
Chalazion is not just an eyelid lump – it is a sign of skin–eyelid–eye microenvironment dysfunction.
Comprehensive care with EYE10, Gel, Naviblef, Spray, MeiboEvacuators, artificial tears, Omega-3 and medication where needed, reduces relapses and protects eyelashes and eyes
Give your eyes the care they deserve with the complete Ophthalmogen line.