When allergies are controlled, but your eyes continue to suffer
You take your antihistamine. Your allergy symptoms are under control. And yet, your eyes are:
• red
• dry or irritated
• tired
• sometimes watering and sometimes feeling tight or “gritty”
If this sounds familiar, you’re not imagining it. And you’re not doing anything wrong.
What is Antihistamine-Induced Dry Eye? (Dry eye caused by antihistamines)?
Antihistamine-induced dry eye is a form of dry eye disease that:
• appears, or
• worsens
in people who take antihistamines for long periods of time.
It does not mean that:
•the medication is “bad”
•your treatment is failing
It means that while antihistamines control allergic inflammation, they can disrupt the eye’s natural lubrication system.
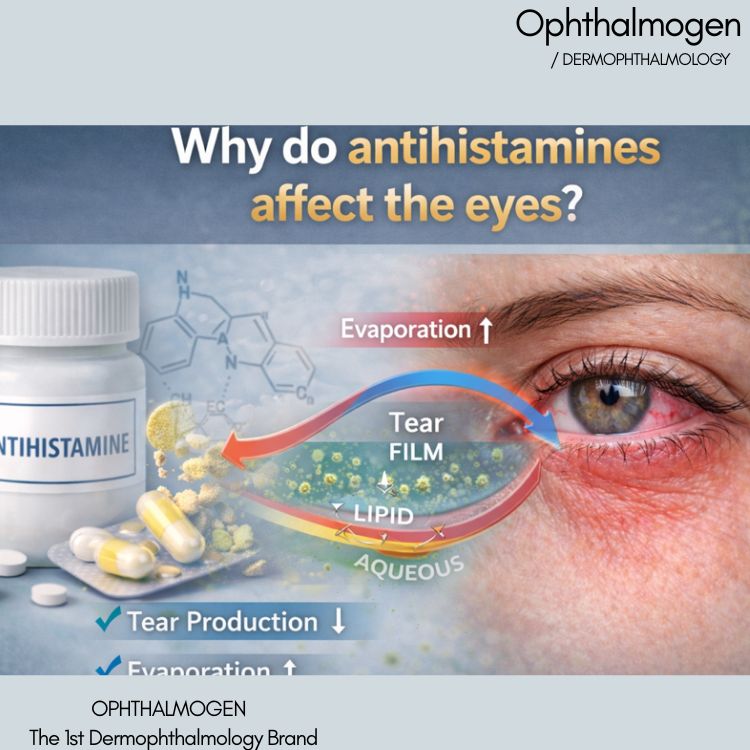
Why can antihistamines affect the eyes?
Antihistamines block H1 histamine receptors. These receptors are not found only in the nose or lungs, but also in:
•the lacrimal (tear) glands
•the eyelids
•the meibomian glands
•the ocular surface
Studies show that antihistamines may:
• reduce tear production
•increase tear evaporation
•impair eyelid function
•destabilize the tear film
That is why eye symptoms may worsen even as allergy symptoms improve.
“I don’t have dry eye – my eyes are watering”
This is one of the most common misunderstandings. Many patients with antihistamine dry eye experience:
• tearing
• sensitivity to wind or air conditioning
•tearing while driving or using screens
This is called paradoxical tearing.
Tears are present, but they are poor quality and evaporate quickly.
The eye overreacts, but remains inadequately protected.
It’s not about “not having enough tears”
According to the international scientific consensus TFOS DEWS II: The most common cause of eye redness and discomfort is not lack of tears, but evaporative dry eye.
In other words:
•tears are present
•but they do not last
And this brings us to the real key player
The root of the problem: the eyelids
Eyelids are not simply “skin around the eye.”
•they host the Meibomian glands
•produce the lipid layer of the tear film
•regulate tear film stability
•protect the eye with every blink
When eyelid function is impaired:
•tears evaporate faster
•blood vessels dilate
•eyes become red, tired, and uncomfortable
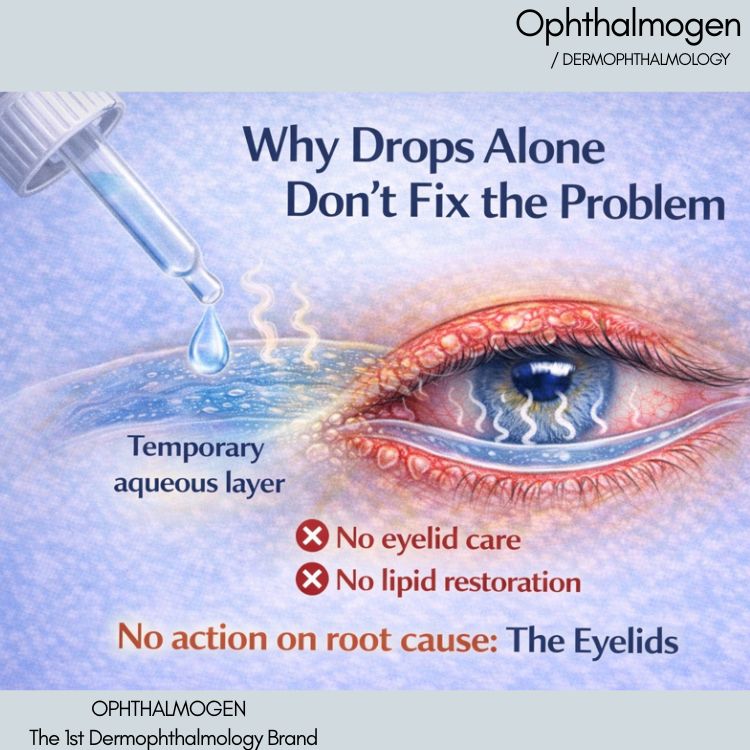
Why artificial tears are often not enough
Artificial tears:
•provide temporary hydration
•offer short-term relief
However
•they do not clean the eyelids
•they do not improve gland function
•they do not restore lipid balance
That is why relief is often short-lived.
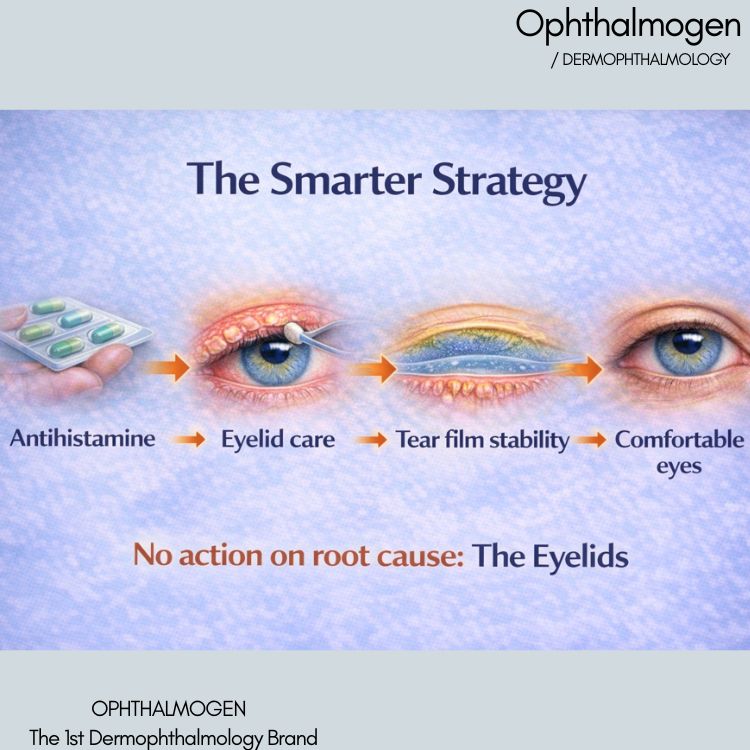
The modern approach: eyelid care
- Dermophthalmology αντιμετωπίζει το μάτι ως ενιαίο σύστημα: βλέφαρα – βλεφαρίδες – οφθαλμική επιφάνεια. Για άτομα που λαμβάνουν αντιισταμινικά:
- daily eyelid care is not a luxury
- it is preventive care for comfortable eyes
What to remember
• Antihistamines are essential for many people
• Dry eye is a known and manageable side effect
• Red eyes do not always mean allergy or infection
• Eyelids play a central role in eye comfort
• Long-term relief requires more than eye drops
When should you see a doctor?
Consult an ophthalmologist if you experience:
• eye pain
• light sensitivity
• discharge
• sudden vision loss
For dryness, redness, and discomfort related to antihistamine use, early supportive care can make a significant difference.
In Summary
Antihistamines are not “bad”. But they are not enough on their own for eye health. Dry eye is an expected side effect. Eyelid care is supported by scientific evidence. Quality of life can improve substantially